Oxytocics and tocolytics in obstetrics
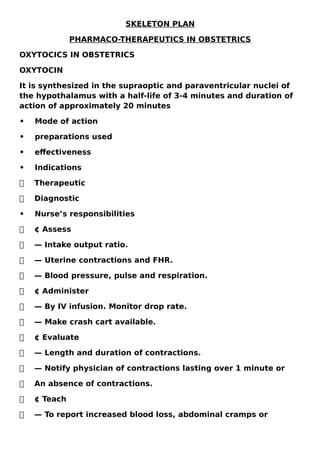
- 1. SKELETON PLAN PHARMACO-THERAPEUTICS IN OBSTETRICS OXYTOCICS IN OBSTETRICS OXYTOCIN It is synthesized in the supraoptic and paraventricular nuclei of the hypothalamus with a half-life of 3-4 minutes and duration of action of approximately 20 minutes • Mode of action • preparations used • effectiveness • Indications Therapeutic Diagnostic • Nurse’s responsibilities ¢ Assess — Intake output ratio. — Uterine contractions and FHR. — Blood pressure, pulse and respiration. ¢ Administer — By IV infusion. Monitor drop rate. — Make crash cart available. ¢ Evaluate — Length and duration of contractions. — Notify physician of contractions lasting over 1 minute or An absence of contractions. ¢ Teach — To report increased blood loss, abdominal cramps or
- 2. Increased temperature. ERGOT DERIVATIVES ¢Mode of action: Ergometrine acts directly on the myometrium ¢ Effectiveness It is highly effective in hemostasis ¢ Indications: — Therapeutic: To stop the atonic uterine bleeding following delivery, abortion or expulsion of hydatidiform mole. — Prophylactic: Against excessive haemorrhage following delivery. CONTRAINDICATIONS: Prophylactic: ¢ Suspected plural pregnancy. ¢ Organic cardiac diseases. ¢ Severe pre-eclampsia and eclampsia ¢ Rh- negative mother. Therapeutic: ¢ Heart disease or severe hypertensive disorders Hazards: ¢ Common side effects are nausea and vomiting. ¢ Precipitate rise in blood pressure, myocardial infarction, stroke and bronchospasm because of vasoconstrictive effect. ¢ Prolonged use may result in gangrene formation of the toes.
- 3. ¢ Prolonged use in puerperium may interfere with lactation PROSTAGLANDINS Mechanism of action ¢PGF2α promotes myometrium contractility ¢PGE2 helps the cervical maturation Contraindications: ¢ Hypersensitivity to the compound. ¢ Uterine scar. Preparations ¢ Tablet. ¢ Vaginal suppository ¢ Vaginal pessary ¢ Prostin E2. ¢ Parenteral Use in obstetrics ¢ Induction of abortion. ¢ Termination of molar pregnancy. ¢ Induction of labour. ¢ Cervical ripening prior to the induction of abortion or labour. ¢ Acceleration of labour. ¢ Management of atonic PPH. ¢ Medical management of tubal ectopic pregnancy. ANTI-HYPERTENSIVE THERAPY METHYLDOPA
- 4. Mechanism of action ¢ -Drugs of the first choice ¢ -Central and peripheral anti-adrenergic action ¢ -Effective and safe for both mother and fetus. Contraindications ¢ -hepatic disorders ¢ -psychic patients ¢ -CCF Dose ¢ -orally 250mg bid may be increased to 1 gm tid depending upon the response. ¢ -IV infusion 250-500mg Side effects -maternal: ¢ postural hypotension ¢ haemolytic anaemia ¢ sodium retention ¢ excessive sedation ¢ coomb’s test may be positive. -fetal: ¢ intestinal ileus LABETALOL Mechanism of action ¢ Combined alpha and beta-adrenergic blocking agents. Contraindication ¢ hepatic disorders. Dose
- 5. ¢ orally: 100mg tid. Maybe increased up to 800 mg daily. ¢ -IV infusion [hypertensive crisis] 1-2 mg/mt until desired effect Side effects ¢ Experience is less compared to methyldopa. efficacy and safety with short-term use. Appear equal to methyldopa. PROPRANOLOL • Mechanism of action • ¢ Beta-adrenergic receptor blocker • Contraindication • ¢ bronchial asthma. • ¢ renal insufficiency. • ¢ diabetes. • ¢ Cardiac failure • ¢ The drug is better avoided for long-term therapy • during pregnancy. • Dose • ¢ orally: 80-120 mg in divided doses Side effects maternal: ¢ severe hypotension ¢ sodium retention ¢ Bradycardia ¢ Bronchospasm ¢ CCF ¢ hypoglycaemia. fetal:
- 6. ¢ bradycardia and impaired fetal responses to hypoxia, IUGR when began in I and II trimesters. -neonatal: hypoglycaemia HYDRALAZINE Mechanism of action ¢ Arteriolar vasodilator. Contraindication ¢ Because of the variable sodium retention, diuretics should be used. Dose ¢ orally: 100mg/day in 4 divided doses. ¢ - IV: 5mg bolus followed by 25g in 200 ml NS at a rate of 2.5 mg/hr to be doubled every 30 mts. Side effects ¢ -maternal: hypotension, tachycardia, arrhythmia, palpitation, lupus-like syndrome. ¢ -fetal: reasonably safe. ¢ -neonatal: thrombocytopenia NIFEDIPINE Mode of action: ¢ Direct arteriolar vasodilation. Dose: ¢ Orally 5-10 mg TID. Contraindications: ¢ Simultaneous use of magnesium sulphate could be hazardous due to synergic effect. Side effects:
- 7. ¢ Flushing ¢ Hypotension ¢ Headache ¢ Tachycardia ¢ Inhibition of labour. SODIUM NITROPRUSSIDE Mechanism of action: ¢ Direct vasodilator. Dose: ¢ Orally 6.25 bid. Side effects: ¢ Maternal — Nausea — Vomiting ¢ Fetal — Oligohydramnios — IUGR — Fetal and neonatal renal failure. NITROGLYCERINE Mechanism of action ¢ Release mainly venous but also arteriolar smooth muscles. Dose: ¢ Given as IV infusion 5μg/min. to be increased at every 3-5 min. up to 100μg/min. Side effects: ¢ Tachycardia
- 8. ¢ Headache ¢ Methaemoglobinaemia Diuretics are used in the following conditions during pregnancy. ¢ Pregnancy-induced hypertension with massive oedema. ¢ Eclampsia with pulmonary oedema. ¢ Severe anaemia in pregnancy with heart failure. ¢ Prior to blood transfusions in severe anaemia. ¢ As an adjunct to certain antihypertensive drugs, such as hydralazine or dioxide FUROSEMIDE Mechanism of action ¢ Acts o loop of the Henle by increasing excretion of sodium and chloride. Dose ¢ 40 mg tab, daily following breakfast for 5 days a week. In acute conditions, parentally 40-120 mg daily. Contraindications: ¢ Hypersensitivity HYDROCHLOROTHIAZIDE Mechanism of action: ¢ Acts on distal tubule by increasing excretion of water, sodium, chloride and potassium. It is used in oedema and hypertension.
- 9. Dose: ¢ PO 25-100 mg/day. Side effects: ¢ Polyuria, glycosuria, frequency. ¢ Nausea, vomiting, anorexia. ¢ Rash, urticaria, fever. ¢ Increased creatinine, decreased electrolytes. TOCOLYTIC AGENTS ¢ Betamimetics ¢ prostaglandin synthetase inhibitors ¢ magnesium sulphate ¢ calcium channel blockers ¢ oxytocin receptor antagonists ¢ nitric oxide donors ¢ antibiotics. BETAMIMETICS • Commonly used drugs: • ¢ Terbutaline • ¢ Ritodrine • ¢ Isoxsuprine • Mechanism of action: • ¢ Activation of the intracellular enzymes [adenylate • cyclase, cAMP, protein kinase] reduces intracellular • free calcium [Ca++] and inhibits the activation of MLCK Dose: ¢ Ritodrine is given by IV infusion, 50μg/min. and increased by 50μg every 10 min. until contractions
- 10. cease. The maximum dose of 350μg/ min. may be given. Infusion is continued for about 12 hours after contraction ceases. ¢ Terbutaline has the longer half-life and has fewer side effects. Subcutaneous injection of 0.25 mg every 3-4 hours is given. ¢ Isoxsuprine has given an IV drip 100 mg in 5D. Rate 0.2 μg/minute. To continue for at least 2 hours after contraction ceases. Maintenance is by IM 10mg six hourly for 24 hours, tab 10 mg 6-8 hourly. INDOMETHACIN Mechanism of action: ¢ Reduces synthesis of PGs thereby reduces intracellular free Ca++, activation of MLCK and uterine contractions. Dose: ¢ Loading dose, 50 mg P.O. or .P.R. followed by 25mg every 6 hrs for 48 hours. Side effects: ¢ Maternal ¢ Heartburn ¢ G.I. bleeding ¢ Asthma ¢ Thrombocytopenia ¢ Renal injury. CALCIUM CHANNEL BLOCKERS • ¢ Nifedipine • ¢ Nicardipine
- 11. • Mechanism of action: • ¢ Nifedipine blocks the entry of calcium inside the cell. • Compared to β- mimetics, effects are less. It is • equally effective to MgSO4. • Dose: • ¢ Oral 10-20 mg every 6-8 hours. MAGNESIUM SULPHATE Mechanism of action: ¢ inhibition of calcium ion Contraindications: ¢ Myasthenia gravis ¢ Impaired renal function Dose: ¢ Loading dose: 4-6 gm I.V. over 20-30 min. followed by an infusion of 1-2 gm/hr to continue tocolysis for 12 hours after contractions have stopped. Side effects: ¢ Maternal ¢ Flushing ¢ Perspiration ¢ Headache ¢ Muscle weakness ¢ Pulmonary oedema rarely ¢ Neonatal ¢ Lethargy ¢ Hypotonia ¢ Respiratory depression rarely.
- 12. OXYTOCIN ANTAGONISTS: ¢ Atosiban Mechanism of action: ¢ It blocks myometrial oxytocin receptors. Dose: ¢ I.V.infusion 300μg/min. the initial bolus may be needed. Side effects: ¢ Nausea ¢ Vomiting ¢ Chest pain ANTICONVULSANTS 1. MAGNESIUM SULPHATE: ¢ Mode of action: ¢ It decreases the acetylcholine release from the nerve endings. ¢ Dose: ¢ IM – loading dose: 4 gm IV [20% solution] over 3-5 min. to follow 10 gm deep IM, 5gm in each buttock. Maintenance dose: 5gm deep IM on alternate buttocks every 4 hrs. ¢ IV- loading dose: 4-6 gm IV over 15-20 min. maintenance dose: 1-2 gm/hr. IV infusion.Side effects: ¢ MgSO4 is relatively safe and is the drug of choice. Muscular paresis[ diminished knee jerks], respiratory failure. Renal function to be monitored. Antidote: ¢ Injection of calcium gluconate 10% 10 ml IV.
- 13. DIAZEPAM mode of action: ¢ central muscle relaxant and anticonvulsant. Dose: ¢ 20-40 mg IV Side effects: ¢ Maternal: ¢ Hypotension ¢ Fetal ¢ Respiratory depression ¢ Hypotonia ¢ Thermoregulatory problem PHENYTOIN Mode of action: ¢ Centrally acting anticonvulsant Dose: ¢ 10 mg/ kg IV at the rate not more than 50 mg/ min followed 2 hrs later by 5 mg/kg. In epilepsy 300- 400 mg daily orally in divided doses. Side effects: ¢ Maternal ¢ Hypotension ¢ Cardiac arrhythmias ¢ Phlebitis at the injection site. ¢ Fetal ¢ Fetal hydantoin syndrome
- 14. ANTICOAGULANTS: HEPARIN Mechanism of action: ¢ It inhibits the action of thrombin Dose: ¢ 5000-10000 I.U. to be administered parenterally [SC or IV]. ¢ Low molecular weight heparin is 2500 IU Side effects: ¢ Maternal: ¢ Haemorrhage ¢ Urticarial ¢ Thrombocytopenia ¢ Osteopenia. ¢ Fetal ¢ It does not cross the placenta WARFARIN Mechanism of action: ¢ Interferes with synthesis of vit K dependent factors. Dose: ¢ 10 mg orally Side effects: ¢ Maternal ¢ Haemorrhage ¢ Fetal ¢ Contradi’s syndrome [skeletal and facial anomalies]
- 15. ¢ Optic atrophy ¢ Microcephaly ¢ Chondrodysplasia punctate. ANALGESIA AND ANAESTHESIA IN OBSTETRICS 1. SEDATIVES AND ANALGESICS ¢ OPIOID ANALGESICS: ¢ PETHIDINE Mechanism of action: ¢ Inhibits ascending pain pathways in CNS, increase pain threshold and alters pain perception. Indications: ¢ Moderate to severe pain in labour, postoperative pain, abruption placentae, pulmonary oedema. Dose: ¢ Injectable preparations contain 50mg/ml can be administered SC, IM, IV. Its dose is 50-100 mg IM combined with promethazine. PETHIDINE Contraindications: Should not be used IV within 2 hrs and IM within 3 hrs of an expected time of delivery of the baby, for fear of birth asphyxia. It should not be used in cases of preterm labour and when the respiratory reserve of the mother is reduced Side effects: ¢ Maternal ¢ Drowsiness ¢ Dizziness
- 16. ¢ Confusion ¢ Headache ¢ Sedation ¢ Nausea ¢ Vomiting ¢ Fetal ¢ Respiratory depression ¢ Asphyxia FENTANYL Mechanism of action: ¢ Inhibits ascending pathways in CNS, increases pain threshold and alters pain perception. Indications: ¢ Moderate to severe pain in labour, postoperative pain an adjunct to the general anaesthetic. Dose: ¢ 0.05 to 0.1 mg IM q1-2 hrs prn. Available in injectable form, 0.05 mg/ml. ¢ Side effects: ¢ Dizziness ¢ Delirium ¢ Euphoria ¢ Nausea ¢ Vomiting ¢ Muscle rigidity ¢ Blurred vision PENTAGON
- 17. • ¢ dose of 30-40 mg • ¢ Naloxone is an efficient and reliable antagonist. • Adverse effects • ¢ Neonate respiratory depression secondary to the • medication crossing the placenta and affecting • the fetus. • ¢ Unsteady ambulation of the client. • ¢ Inhibition of the mother’s ability to cope with the • the pain of labour. Tranquillizers • ¢ DIAZEPAM: Usual dose is 5-10 mg. • ¢ MIDAZOLAM: Dose of 0.05 mg/kg is given • intravenously • ¢ COMBINATION OF NARCOTICS AND • Tranquillizers • ¢ BUTORPHANOL and NALBUPHINE INHALATIONAL METHODS • ¢ Nitrous oxide and air • ¢ Premixed nitrous oxide and oxygen • ¢ Trichloroethylene • ¢ Methoxyflurane, isoflurane, enflurane EPIDURAL AND SPINAL REGIONAL ANALGESIA • Adverse effects • ¢ nausea and vomiting. • ¢ Inhibition of bowel and bladder elimination • sensations.
- 18. • ¢ Bradycardia or tachycardia. • ¢ Hypotension. • ¢ Respiratory depression. • ¢ Allergic reaction and pruritus. PUDENDAL BLOCK It consists of a local anaesthetic such as lidocaine(Xylocaine) or bupivacaine (Marcaine) being administered transvaginally into the space in front of the pudendal nerve. EPIDURAL ANAESTHESIA • The epidural block consists of a local anaesthetic bupivacaine (Marcaine) along with an analgesic morphine (Duramorph) or fentanyl (Sublimaze) injected into the epidural space at the level of the fourth or fifth vertebrae. • Adverse effects • Maternal hypotension. • Fetal bradycardia. • Inability to feel the urge to void. • Loss of the bearing down reflex. SPINAL BLOCK • The spinal block consists of a local anaesthetic injected into the subarachnoid space into the spinal fluid at the third, fourth, or fifth lumbar interspace, alone or in combination with an analgesic such as fentanyl. • Adverse effects • Maternal hypotension. • Fetal bradycardia. • Loss of the bearing down reflex. PARACERVICAL BLOCK
- 19. • It consists of lidocaine (Xylocaine) being injected into the cervical mucosa early in labour during the first stage to block the pain of uterine contractions. • Adverse effects include fetal bradycardia. • Improper technique can result in serious toxicity. GENERAL ANAESTHESIA • 100% oxygen is administered by tight mask fit for more than 3 minutes. • Induction of anaesthesia is done with the injection of thiopentone sodium 200- 250 mg as a 2.5 % solution IV., followed by refrigerated suxamethonium 100 mg. • the patient is intubated with cuffed ET tube. • Anaesthesia is maintained with 50% NO2, 50% oxygen and a trace of halothane. • Relaxation is maintained with non-depolarizing muscle relaxant [ vecuronium 4 mg or atracurium 25 mg]. FETAL HAZARDS ON MATERNAL MEDICATION DURING PREGNANCY • Mechanism of teratogenicity • ¢Folic acid deficiency. • ¢Epoxides or arena oxides • ¢Environmental and genes • abnormalities. • ¢Maternal disease and drugs • ¢Homebox genes Maternal-fetal drug transfer and the hazards • ¢ before D 31: • Teratogen produces an all or none effect. • ¢ D31-d71:
- 20. • It is the critical period for organ formation. • ¢ After D 71: • The development of other organs continues. MATERNAL DRUG INTAKE AND BREASTFEEDING Transfer of drugs through breast milk depends on following factors: ¢ Chemical properties ¢ Molecular weight ¢ Degree of protein binding ¢ Ionic dissociation ¢ Lipid solubility ¢ Tissue pH. ¢ Drug concentration. ¢ Exposure time. DRUGS IDENTIFIED AS HAVING EFFECT ON LACTATION AND THE NEONATE ¢ Bromide: Rash. Drowsiness, and poor feeding. ¢ Iodides: Neonatal hypothyroidism ¢ Chloramphenicol: Bone marrow toxicity ¢ Oral pill: Suppression of lactation. ¢ Bromocriptine: Suppression of lactation. ¢ Ergot: Suppression of lactation. ¢ Metronidazole: Anorexia, blood dyscrasias, irritability, weakness, neurotoxic disorders. ¢ Anticoagulants: Haemorrhagic tendency.
- 21. ¢ Isoniazid: Anti-DNA activity and hepatotoxicity. ¢ Anti-thyroid drugs and radioactive iodine: Hypothyroidism and goitre, agranulocytosis. ¢ Diazepam, opiates, phenobarbitone: Sedation effect with the poor sucking reflex.
