Presentation1.pptx, ultrasound examination of the neonatal head.
- 1. Dr/ ABD ALLAH NAZEER. MD. Ultrasound examination of the neonatal head.
- 2. ULTRASOUND OF THE NEONATAL HEAD PROTOCOL INDICATIONS Prematurity: Some people discriminate between the terms preterm and premature. Preterm refers to delivering prior to 37weeks whilst a premature infant is one that has not yet reached the level of fetal development that generally allows life outside the womb. The fine network of vessels (the germinal matrix) on the floor of the anterior horn of the lateral ventricles (the ependyma) are extremely fragile. If there is any hypoxic episode, the reactive increase in blood pressure can result in a hemorrhage of these vessels. Usually assessed at day 1 and again at day 7. Increased head circumference Persisting large fontanelle Craniosynostosis (premature closure of sutures) Trauma Known hypoxia Follow up of known pathology Failure to thrive Suspected intracranial mass or infection
- 3. LIMITATIONS If the anterior fontanel is very small or closed your visibility will be reduced or completely obscured. Even with a large fontanelle, the peripheral extremes of the brain are obscured from view. EQUIPMENT SELECTION AND TECHNIQUE Probes: Primarily a small footprint, wide sector, mid.-frequency probe is essential. Ideally a specific 5-8MHz vector probe however a trans-vaginal probe also provides excellent imaging. (A TV probe can be ergonomically difficult to use for some operators and awkward to ft in a humidicrib.) You may also require a high frequency linear array to assess superficial structures and a curvilinear probe for axial trans-temporal images. Environment: A warm room with warm gel. If still in high oxygen environment, this should be maintained as much as possible. Patient position: If still in a humidicrib as a high oxygen environment, the baby must be scanned there. You may need to place a cloth under and/or beside the baby's head to support and immobilize it for the scan.
- 4. SCANNING TECHNIQUE Use sufficient gel to not require too much transducer pressure. Approach is generally via the anterior fontanel. The posterior fontanel can also be used. Using the small footprint sector or TV probe: Begin in a coronal plane slowly sweeping from the anterior to the posterior. Rotate 90o to perform sagittal and para-sagittal views. Using the high frequency linear probe: Gently scan through the anterior fontanelle in transverse. You should assess the superior sagittal sinus for patency, and the sub-arachnoid space. You will usually be able to scan as deep as the 3rd ventricle. Using the 5mHz curvilinear probe: scan through the temple in an axial plane, particularly assessing the opposite subdural region.
- 5. WHAT TO LOOK FOR: A solid grasp of the intracranial anatomy is vital. Also, a thorough understanding of the developmental evolution of the neonatal brain and how it changes between 28weeks and term. Essentially, the normal 10week premature brain is relatively smooth, homogenous & devoid of sulci/gyrae. SAGITTAL Midline (must include corpus callosum the 3rd and 4th ventricles and cerebellum). Parasagittal to show caudothalamic notch and detail of lateral venticles Far lateral to show periventricular white matter. CORONAL frontal caudate region series of images caudate to trigone of lateral ventricles occipital region MEASUREMENTS Coronal: frontal horn of lateral ventricles at the foramen of Monroe (caudate nucleus) Sagittal: trigone of lateral ventricles
- 6. ULTRASOUND OF THE NEONATAL HEAD - Normal Normal sagittal at the 3rd and 4th ventricles. Normal anterior coronal neonatal brain. Scan, angling forward of this point as far as possible to the 'bulls-horns' of the sphenoid bone.
- 7. Normal parasagittal at the lateral ventricles. Normal mid-anterior coronal at the sylvian fissures and 3rd ventricle.
- 8. Normal far-posterior coronal. Normal mid coronal view at the level of the brain stem.
- 9. Normal coronal view of the lateral ventricles and caudao-thalamic groove. Normal posterior coronal using a linear array transducer. Zoomed at the level of the trigone of the lateral venticles, visualizing the body of the choroid plexii.
- 10. The superior sagittal sinus and other vascular channels can be readily assessed with power Doppler. Normal far-posterior coronal.
- 11. Coronal images for neonatal brain, C (caudate), T (thalamus),F (foramen of Monro), m (midbrain), 3 (third ventricle), q(quadrigeminal plate cistern), CB(cerebellar hemispheres.
- 12. Sagittal images for neonatal brain, 3 (third ventricle), mi(mass intermedia), p(pelly of pons), 4 (fourth ventricle), cv (cerebellar vermis), C(caudate nucleus), t(thalamus).
- 14. Germinal Matrix Hemorrhage Germinal matrix hemorrhage (GMH) is also known as periventricular hemorrhage or preterm caudothalamic hemorrhage. These germinal matrix hemorrhages occur in the highly vascular but also stress sensitive germinal matrix, which is located in the caudothalamic groove. This is the subependymal region between the caudate nucleus and thalamus. The germinal matrix is only transiently present as a region of thin-walled vessels, migrating neuronal components and vessel precursors It has matured by 34 weeks gestation, such that hemorrhage becomes very unlikely after this age. Most GMHs occur in the first week of life Most common in infants These hemorrhages start in the caudothalamic groove and may extend into the lateral ventricle and periventricular brain parenchyma. Most infants are asymptomatic or demonstrate subtle signs that are easily overlooked. These hemorrhages are subsequently found on surveillance sonography.
- 16. Grade 1 intracranial hemorrhage, Sagittal and coronal US of subependymal hemorrhage located in the groove between the thalamus and the nucleus caudatus.
- 18. Coronal section - grade I - subependymal germinal matrix hemorrhage (blue arrows).
- 20. Sagittal and coronal US of a grade 2 hemorrhage.
- 21. Coronal section - grade II - GMH and IVH without ventricular dilation (blue arrow).
- 23. LEFT: Coronal image, green arrow indicating grade 3 hemorrhage RIGHT: Sagittal image, yellow arrow indicating venous infarction.
- 24. Sagittal section - grade III - GMH and IVH with ventricular dilation (white arrows).
- 27. Peri Ventricular Leukomalacia (PVL) PVL is also known as Hypoxic-Ischemic Encephalopathy (HIE) of the preterm. It is a white matter disease that affects the periventricular zones. In prematures this white matter zone is a watershed zone between deep and superficial vessels. Until recently ischemia was thought to be the single cause of PVL, but probably other causes (infection, vasculitis) play an additional role. PVL presents as areas of increased periventricular echogenicity. Normally the echogenicity of the periventricular white matter should be less than the echogenicity of the choroid plexus. PVL occurs most commonly in premature infants born at less than 33 weeks gestation (38% PVL) and less than 1500 g birth weight (45% PVL). Detection of PVL is important because a significant percentage of surviving premature infants with PVL develop cerebral palsy, intellectual impairment or visual disturbances. More than 50% of infants with PVL or grade III hemorrhage develop cerebral palsy.
- 30. Sagittal image of a child with PVL grade 1.
- 31. Transverse and sagittal image of a child with PVL grade 2.
- 32. Sagittal and coronal images demonstrating extensive PVL grade 3
- 33. Coronal and transverse images demonstrating PVL grade 4.
- 34. Coronal and transverse images demonstrating PVL grade 4.
- 37. Aneurysm of vein of Galen.
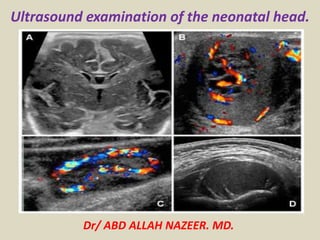
- 38. Gray-scale and Doppler coronal USG demonstrating a cystic midline structure in the region of posterior third ventricle with mass effect. (A) Typical swirl effect is noted on Doppler (B). Findings are highly suggestive of aneurysmal malformation of the vein of Galen. The corresponding axial and sagittal T2W images of MR examination confirming large aneurysmal dilatation of the vein of Galen (C and D)
- 41. Coronal section - Absent corpus callosum, widely separated frontal horns of lateral ventricles, dilation and posterosuperior displacement of third ventricle. Partial agenesis corpus callosum.
- 46. Coronal section - Dandy - Walker malformation - dilation of the fourth ventricle (blue star), hypoplastic cerebellar hemispheres.
- 48. Porencephalic cyst: Large foci of intraventricular/intraparenchymal bleed could lead to a cavitating destructive lesion in the brain parenchyma. After resolution and evacuation of the hematoma, the cavity of the lesion communicates with the ventricular system, leading to the formation of a porencephalic cyst. Porencephalic cysts, which are, often, a sequel of grade 4 hemorrhages are usually associated with higher neurodevelopmental defects . Coronal USG and the high-resolution parasagittal view demonstrating a large porencephalic cyst communicating with the left lateral ventricular cavity.
- 52. Choroid plexus cysts. Common, 3% prevalence. Glomus. < 1cm, unilateral = insignificant. > 1cm, bilateral = increase associated with chromosomal abnormalities.
- 53. Midline cystic structures. Communicate with each other. Do not communicate with ventricular system or subarachnoid spaces. Obliterated from posterior to anterior.
- 54. Cavum septum pellucidum and vergue.
- 57. Connatal Cysts. Normal variant: incidence = 0.7%. Superolateral to frontal horns. Anterior to Foramen of Monroe. String of pearls. Resolve spontaneously.
- 59. Caudothalamic Groove Cysts. Congenital: Germinolytic. Chromosomal, metabolic, incidental Acquired: Subependymal Post-hemorrahgic
- 61. Benign Hygroma of infancy. Children 6 months to 2 years. Head circumference > 97th percentile Cause unknown, ? Familial. Subarachnoid spaces > 3.3 mm +/_ slight ventricular enlargement
- 62. Benign Hygroma
- 63. Hydrocephalus. Obstructive: non-communicating). Most common. CSF cannot enter subarachnoid space Aqueductal stenosis, Chiari Malformation, Dandy-Walker. Non-obstructive: communicating). Impaired CSF resorption. Infection, hemorrhage, congenital absence arachnoid villi. Ex Vacuo: Loss of brain parenchyma lead to increase CSF spaces.
- 64. Mild to moderate Hydrocephalus.
- 65. Mild Hydrocephalus. Moderate to marked Hydrocephalus.
- 66. Coronal section - Hydrocephalus with little ventricular dilation (blue stars). Coronal section – Large hydrocephalus (blue star).
- 67. Aqueductal stenosis causing obstructive hydrocephalus.
- 68. Coronal and parasagittal USG demonstrating colpocephaly in a patient with agenesis of corpus callosum. Also, there is hypoplasia of the cerebellum, mainly involving the right lobe
- 69. Holoprosencephaly: Ultrasound may also show a snake under the skull sign in some situations. Holoprosencephaly is a rare congenital brain malformation resulting from incomplete separation of the two hemispheres. Alobar holoprosencephaly In alobar holoprosencephaly, the thalami are fused and there is a single large posteriorly located ventricle. Most commonly associated with facial abnormalities such as cyclopia, ethmocephaly, cebocephaly, and median cleft lip. For more details see the article on alobar holoprosencephaly Semilobar holoprosencephaly Here the basic structure of the cerebral lobes are present, but are fused most commonly anteriorly and at the thalami. The olfactory tracts and bulbs are usually not present, and there is agenesis or hypoplasia of the corpus callosum. For more details see the article on semilobar holoprosencephaly Lobar holoprosencephaly This is the least affected subtype. Patients demonstrate more subtle areas of midline abnormalities such as fusion of the cingulate gyrus and thalami. The olfactory tracts are absent or hypoplastic. There may be hypoplasia or absence of the corpus callosum.
- 72. Coronal section - Alobar holoprosencephaly - large, horseshoe-shaped single ventricular cavity (blue arrow) and fused thalami (pink star).
- 75. Hydranencephaly is a rare encephalopathy that occurs in-utero. It is characterised by destruction of the cerebral hemispheres with transformation of the same into a membranous sac containing cerebrospinal fluid and the remnants of cortex and white matter . Hydranencephaly.
- 76. Hydranencephaly.
- 77. Anencephaly is the most severe form of cranial neural tube defect (NTD) and is characterised by absence of cortical tissue (although brainstem and cerebellum may be variably present) as well as absence of the cranial vault. Morphological spectrum within anencephaly ranges from holocrania (severest form) to merocrania (mildest form) Antenatal ultrasound Anencephaly may be sonographically detectable as early as 11 weeks. Ultrasound can be a non invasive, cost effective and fast method to detect anencephaly and has an accuracy of approximating 100% at 14 weeks no parenchymal tissue is seen above the orbits and calvarium is absent: parts of the occipital bone and mid brain may be present if a small amount of neural tissue is present, it is then termed exencephaly this may be seen at an earlier stage less than expected value for crown rump length (CRL) a "frog eye" or "mickey mouse" appearance may be seen when seen in the coronal plane due to absent cranial bone/brain and bulging orbits. may show evidence of polyhydramnios: due to impaired swallowing
- 78. Anencephaly
- 79. Encephalocele (also known as meningoencephalocele) are a type of cephalocoele where brain tissue herniates out through a defect in the cranium. Antenatal ultrasound An encephalocoele may be seen as a purely cystic mass or may contain echoes from herniated brain tissue. if the mass appears cystic, the meningocele component predominates, while a solid mass indicates predominantly an encephalocele. Larger encephalocoeles may show accompanying microcephaly.
- 80. Occipital meningocele with encephalocele
- 81. Coronal section - periventricular calcifications (white arrows) in a patient with CMV infection Sagittal and coronal views - Tuberous sclerosis - marked echogenous intracerebral foci.
- 82. Fetal intracranial hemorrhage may occur either within the cerebral ventricles, subdural space or infratentorial fossa. Antenatal ultrasound The sonographic appearance of fetal intracranial hemorrhage is extremely variable, depending on its location and age of the hemorrhage. A massive intraparenchymal hemorrhage can sometimes be seen as an irregular hyperechoic mass. As the hemorrhage matures, porencephalic cyst formation or fetal intracranial calcification may be seen.
- 83. USG images demonstrating a grade 4 left intracranial hemorrhage. Note extensive ill-defined intraparenchymal component with relatively less mass effect, indicating hemorrhagic venous infarct
- 84. Large right tempo-occipital and cerebellar hemorrhage, shown as the hyperechoic area in the coronal and parasagittal images
- 85. Acute ischemia: Evaluation of diffuse brain edema is technically challenging on neurosonography. As the size of the ventricles varies considerably, ventricular size is unreliable as a parameter in assessing the mass effect. The usual observation in the cases of ischemia is a combination of diffuse increase in the echogenicity of ganglionic areas with associated obliteration of cisterns and small capacity of the ventricles. CT and/or magnetic resonance imaging (MRI) still remain as superior techniques in assessing diffuse intracranial ischemia Serial Doppler examination of the intracranial vessels and circle of Willis is helpful in evaluating the severity of intracranial ischemia. Diastolic flow, reflected in Resistive Index (RI) is a measure that will indicate the hemodynamic status of intracranial flow. Coronal USG at two levels demonstrating the subtle increase in the cerebral parenchymal echoes in a patient with acute ischemia (secondary to meconium aspiration). Note the small-capacity ventricles and obliterated cisternal spaces
- 86. Cerebral edema. Increased parenchyma echogenicity. Decreased sulcal/gyral differentiation. Decrease vascular pulsations.
- 87. Perivascular Mineralization. TORCH. Trisomies(21 and 13). Twin-twin transfusion. Neonatal asphyxia. TORCH infection.
- 88. TORCH infection.
- 89. High-resolution images of the subarachnoid spaces; normal high-convexity subarachnoid space is demonstrated (yellow arrows). (B) Shows a dilated subarachnoid space with internal echoes in a patient with pyogenic meningitis (black arrows)
- 90. Thank You.
