Antidiabetic drug-1
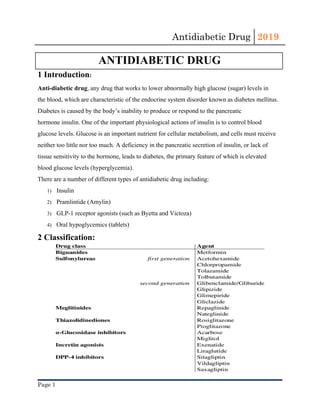
- 1. Antidiabetic Drug 2019 ANTIDIABETIC DRUG 1 Introduction: Anti-diabetic drug, any drug that works to lower abnormally high glucose (sugar) levels in the blood, which are characteristic of the endocrine system disorder known as diabetes mellitus. Diabetes is caused by the body’s inability to produce or respond to the pancreatic hormone insulin. One of the important physiological actions of insulin is to control blood glucose levels. Glucose is an important nutrient for cellular metabolism, and cells must receive neither too little nor too much. A deficiency in the pancreatic secretion of insulin, or lack of tissue sensitivity to the hormone, leads to diabetes, the primary feature of which is elevated blood glucose levels (hyperglycemia). There are a number of different types of antidiabetic drug including: 1) Insulin 2) Pramlintide (Amylin) 3) GLP-1 receptor agonists (such as Byetta and Victoza) 4) Oral hypoglycemics (tablets) 2 Classification: Page 1
- 2. Antidiabetic Drug 2019 2.1 Overview of Antidiabetic drug: Class Mechanism of action Side effects Contraindications Biguanide (metformin) Enhances the effect of insulin Lactic acidosis Weight loss Gastrointestinal complaints are common (e.g. diar rhea, abdominal cramps) Reduced vitamin B12absorption Chronic kidney disease Liver failure Metformin must be paused before administration of iodinated contrast medium and major surgery. Sulfonylureas (e.g., glyburid e, glimepiride) Increase insulin secr etion from pancreaticβ-cel ls Risk of hypoglycemia Weight gain Hematological changes: agranulo cytosis, hemolysis Severe cardiovascular comorbidity Obesity Sulfonamide allergy (par ticularly long-acting sub stances) Meglitinides (nateglinide, rep aglinide) Increase insulin secr etion from pancreaticβ-cel ls Risk of hypoglycemia Weight gain Severe renal or liver failure DPP-4 inhibitors (saxagliptin, sitagli ptin) Inhibit GLP-1 degra dation → promotes glucose-de pendent insulin secre tion Gastrointestinal complaints Pancreatitis Headache, dizziness Arthralgia Liver failure Moderate to severe renal failure GLP-1 agonists (incretin mimetic drugs: exenatide, liraglutide, albiglutide) Direct stimulation of the GLP-1 receptor Nausea Increased risk of pancreatitisand possibly pancreati c cancer Preexisting, symptomatic gastrointest inal motility disorders Page 2
- 3. Antidiabetic Drug 2019 SGLT-2 inhibitors(canagliflozin, dapa gliflozin, empagliflozin) Increased glucosuria through the inhibition of SGLT-2 in the kidney Genital yeast infe ctions and urinary tract infections Polyuria and dehy dration Diabetic ketoacidosis Chronic kidney disease Recurrent urinary tract infections Alpha-glucosidase inhibitors(acarbose) Reduce intestinal glucose absorption Gastrointestinal complaints (flatulence, diarrh ea, feeling of satiety) Any preexisting intestinal conditions (e.g., inflammatory bowel disease) Severe renal failure Thiazolidinediones(pioglitaz one) Reduce insulin resistance through the stimulation of PPARs (peroxisome proliferator-activated receptors) Increase transcriptio n of adipokines Weight gain Edema Cardiac failure Increased risk of bone fractures (os teoporosis) Congestive heart failure Liver failure Amylin analogs (pramlintide) Reduce glucagon rel ease Reduce gastric emptying Increase satiety Risk of hypoglycemia Nausea Gastroparesis 3 Common contraindications of antidiabetic agents ● Type 1 diabetes mellitus: Patients require insulin therapy (see principles of insulin therapy). ● Pregnancy and breastfeeding (also see gestational diabetes): All antidiabetic agents are contraindicated. Antidiabetic drugs should be substituted with human insulin as early as possible (ideally prior to the pregnancy). Page 3
- 4. Antidiabetic Drug 2019 ● Renal failure : Antidiabetic drugs that may be administered if GFR < 30 mL/min include DPP-4 inhibitors, incretin mimetic drugs, meglitinides, and thiazolidinediones. ● Morbidity and surgery. ● Pause antidiabetic treatment in the following cases: ● Major surgery performed under general anesthesia. ● Acute conditions requiring hospitalization (infections, organ failure). ● Elective procedures associated with an increased risk of hypoglycemia (periods of fasting, irregular food intake). 4 Insulinotropic agents ● Mechanism: stimulate the secretion of insulin from pancreatic β-cells. ● Glucose-independent: Insulin is secreted regardless of the blood glucose level, even if blood glucose levels are low → risk of hypoglycemia. ● Sulfonylurea, meglitinides. ● Glucose-dependent: Insulin secretion is stimulated by elevated blood glucose levels (postprandially). These antidiabetic agents depend on residual β-cellfunction. ● GLP-1 agonists, DPP-4 inhibitors. 5 Non-insulinotropic agents ● Mechanism:These agents do not depend on residual insulin production. ● Effective in patients with nonfunctional endocrine pancreatic β-cells.. ● Biguanides (metformin), SGLT-2 inhibitor, thiazolidinediones, alpha-glucosidase inhibitors. 5.1 Biguanides (Metformin) 5.1.1 Mechanism of action: ● enhances the effect of insulin. ● Reduction in insulin resistance via modification of glucose metabolic pathways. ● Inhibits mitochondrial glycerophosphate dehydrogenase (mGPD).. ● Decreases hepatic gluconeogenesis and intestinal glucose absorption. ● Increases peripheral insulin sensitivity. Page 4
- 5. Antidiabetic Drug 2019 ● Lowers postprandial and fasting blood glucose levels. ● Reduces LDL, increases HDL. 5.1.2 Indications: drug of choice in all patients with type 2 diabetes. 5.1.3 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 1.2–2% over 3 months. ● Weight loss or weight stabilization. ● No risk of hypoglycemia. ● Beneficial effect on dyslipidemia. ● Studies show metformin reduces the risk of macroangiopathic complications in diabetic patients. ● Cost-effective. 5.1.4 Important side effects: ● Metformin-associated lactic acidosis. ● Incidence: ∼ 8 cases/100,000 patient years. ● Clinical features: frequently nonspecific. ● Gastrointestinal prodromal symptoms: nausea, vomiting, diarrhea, abdominal pain. ● Severe symptoms: muscle cramps, hyperventilation, apathy, disorientation, coma. Page 5
- 6. Antidiabetic Drug 2019 ● High-risk groups. ● Elderly individuals. ● Patients with cardiac or renal insufficiency. ● Diagnostics. ● Arterial blood gas (ABG): metabolic acidosis and anion gap. ● ↑ Serum lactate. ● Treatment: discontinue metformin and treat acidosis. ● Gastrointestinal complaints are common: nausea, diarrhea, flatulence. ● Vitamin B12 deficiency. ● Metallic taste in the mouth (dysgeusia). 5.1.5 Contraindications: ● Renal failure (if creatinine clearance < 30 mL/min). ● Severe liver failure. ● Intravenous iodinated contrast medium. ● Pause metformin prior to surgery. ● Chronic pancreatitis, starvation ketosis, ketoacidosis, sepsis. ● Heart failure (NYHA III and IV), respiratory failure, shock, sepsis. ● Alcoholism. 5.1.6 Important interactions: sulfonylureas 5.2 Thiazolidinediones (glitazones, insulin sensitizers) 5.2.1 Active agents: ● Pioglitazone ● Rosiglitazone 5.2.2 Mechanism of action: ● Activation of the transcription factor PPARγ (peroxisome proliferator-activated receptor of gamma type). ● ↑ Transcription of genesinvolved in glucose and lipid metabolism. ● ↑ levels of adipokines such as adiponectin. Page 6
- 7. Antidiabetic Drug 2019 ● ↑ Storage of triglycerides and subsequent reduction of products of lipid metabolism (e.g., free fatty acids) that enhance insulin resistance . ● Glucose utilization is increased and hepatic glucose production reduced. 5.2.3 Indications: May be considered as a monotherapy in patients with severe renal failure and/or contraindications for insulin therapy. 5.2.4 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 1% in 3 months. ● Favorable effect on lipid metabolism: ↓ triglyceride, ↓ LDL, ↑ HDL. ● No risk of hypoglycemia. 5.2.5 Important side effects: ● Fluid retention and edema. ● Weight gain. ● Increased risk of heart failure. ● Increased risk of bone fractures (osteoporosis!). 5.2.6 Contraindications: ● Congestive heart failure (NYHA III or IV). ● Liver failure. Page 7
- 8. Antidiabetic Drug 2019 ● Pioglitazone: history of bladder cancer or active bladder cancer; macrohematuria of unknown origin. 5.3 Sulfonylureas 5.3.1 Active agents: ● Glyburide: the standard substance of this class with a relatively long half-life. ● Glipizide: a short-acting agent. 5.3.2 Mechanism of action: ● Sulfonylureas block ATP-sensitive potassium channels of the pancreatic β-cells. ● Depolarization of the cell membrane. ● Calcium influx. ● Insulinsecretion. ● Extrapancreatic effect: decreases hepatic gluconeogenesis and increases peripheral insulin sensitivity. Page 8
- 9. Antidiabetic Drug 2019 5.3.3 Indications: Particularly suitable for patients who are not overweight, do not consume alcohol, and adhere to a consistent dietary routine. 5.3.4 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 1.2% over 3 months. ● Long-term experience. ● Low-cost. 5.3.5 Important side effects: ● Life-threatening hypoglycemia. ● Increased risk in patients with renal failure. ● Weight gain. ● Hematological changes: granulocytopenia, hemolytic anemia. ● Allergic skin reactions. ● Alcohol intolerance. ● Compared to metformin, sulfonylureas are associated with more cardiovascular (macrovascular) complications. 5.3.6 Contraindications: ● Severe cardiovascular comorbidity. ● Obesity. ● Sulfonamide allergy (particularly long-acting substances). ● Severe liver failure. ● Severe kidney failure. 5.4 Meglitinides (sulfonylurea analogue) 5.4.1 Active agents: ● Repaglinide: the leading agent in the class of meglitinides, which is well tolerated by patients with chronic kidney disease ● Nateglinide Page 9
- 10. Antidiabetic Drug 2019 5.4.2 Mechanism of action: ● Enhances insulin secretion (similar mechanism of action to that of the sulfonylureas). ● Meglitinides should be taken shortly before meals. 5.4.3 Indications: particularly suitable for patients with postprandial peaks in blood glucose levels. 5.4.4 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 0.75% over 3 months. ● More expensive than sulfonylureas. 5.4.5 Important side effects: ● Life-threatening hypoglycemia (less risky than sulfonylureas). ● Increased risk in patients with renal failure. ● Weight gain. ● Hepatotoxicity (rare). Page 10
- 11. Antidiabetic Drug 2019 5.4.6 Contraindications: ● Severe liver failure. ● Severe renal failure. 5.4.7 Interactions: Sulfonylureas. 5.5 Incretinmimetics (GLP-1 receptor agonists) 5.5.1 Active agents: ● Exenatide. ● Liraglutide: rapid-release formula that is administered daily. ● Albiglutide: extended-release formula that is administered once weekly. ● Dulaglutide. 5.5.2 Mechanism of action: ● Incretin effect: 1. Food intake. 2. Activation of enteroendocrine cells in the gastrointestinal tract. 3. Release of GLP-1. 4. GLP-1 degradation via the enzyme DPP-4. 5. End of the GLP-1 effect. ● Incretin mimetic drugs bind to the GLP-1 receptors and are resistant to degradation by DPP-4 enzyme ● Increase insulin secretion, decrease glucagonsecretion, slow gastric emptying (↑ feeling of satiety, ↓ weight) Page 11
- 12. Antidiabetic Drug 2019 5.5.3 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 0.5–1.5% over 3 months ● Subcutaneous injection ● Weight loss ● No risk of hypoglycemia 5.5.4 Side effects: ● Gastrointestinal complaints (particularly impaired gastric emptying!) ● Increased risk of pancreatitis and potentially pancreatic cancer : 5.5.5 Contraindications: ● Preexisting symptomatic gastrointestinal motility disorders ● Chronic pancreatitis or a family history of pancreatic tumors 5.6 Dipeptidyl peptidase-4 inhibitors (gliptins) 5.6.1 Active agents: ● Sitagliptin ● Saxagliptin 5.6.2 Mechanism of action: Page 12
- 13. Antidiabetic Drug 2019 ● Gliptins indirectly increase the endogenous incretin effect by inhibiting the dipeptidyl peptidase. ● 4 enzyme that breaks down glucagon-like peptide 1. ● Increased insulin secretion, decreased glucagon secretion, delayed gastric emptying. 5.6.3 Indications: Antihyperglycemic therapy algorithm for type 2 diabetes. 5.6.4 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 0.5–0.75% over 3 months.No risk of hypoglycemia unless insulin and/or insulinotropic drugs are used simultaneously. 5.6.5 Important side effects: ● Gastrointestinal complaints: diarrhea, constipation (milder than in GLP-1 agonist exposure). ● Nasopharyngitis and upper respiratory tract infection. ● Arthralgia. ● Headaches, dizziness. ● Urinary infections (mild). ● Increased risk of pancreatitis. ● Acute renal failure. Page 13
- 14. Antidiabetic Drug 2019 5.6.6 Contraindications: ● Hypersensitivity. ● Liver failure. 5.7 SGLT-2 inhibitors (gliflozins) 5.7.1 Active agents: ● Dapagliflozin ● Empagliflozin ● Canagliflozin 5.7.2 Mechanism of action: ● Reversible inhibition of the sodium-dependent glucose co-transporter (SGLT-2) in the proximal tubule of the kidney. ● reduced glucose reabsorption in the kidney. ● glycosuria and polyuria. 5.7.3Indications: A treatment option used especially in young patients with treatment-compliant type 2 DM without significant renal failure. Page 14
- 15. Antidiabetic Drug 2019 5.7.4 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 0.6% over 3 months. ● Promotes weight loss. ● Reduces blood pressure. 5.7.5 Important side effects: ● Urinary tract infections, genital infections (vulvovaginitis, balanitis). ● Dehydration as a result of polyuria. ● Severe diabetic ketoacidosis. 5.7.6 Contraindications: ● Chronic kidney disease. ● Recurrent urinary tract infections (e.g., in patients with anatomical or functional anomalies of the urinary tract). 5.8 Alpha-glucosidase inhibitors 5.8.1 Active agents: ● Acarbose ● Miglitol 5.8.2 Mechanism of action: ● Inhibits alpha-glucosidase. ● Decreased intestinal glucose absorption. ● The drug is particularly effective in controlling postprandial blood glucose levels. ● The undigested carbohydrates reach the colon, where they are degraded by intestinal bacteria, resulting in the production of intestinal gas. Page 15
- 16. Antidiabetic Drug 2019 5.8.3 Clinical characteristics: ● Glycemic efficacy: lowers HbA1c by 0.8% over 3 months. ● No risk of hypoglycemia. 5.8.4 Important side effects: gastrointestinal complaints (flatulence, abdominal discomfort, diarrhea). 5.8.5 Contraindications ● Inflammatory bowel disease. ● Conditions associated with malabsorption. ● Severe renal failure. Page 16
- 17. Antidiabetic Drug 2019 References: 1. https://www.amboss.com/us/knowledge/Antidiabetic_drugs 2. American Diabetes Association. Diabetes Basics. Accessed 11/5/2018 3. MIMS. 2013. [12 December 2013]. Available from: http://www.mims.co.uk/ Page 17