High-Protein Nutrition May Help Manage Diabetes and Blood Sugar
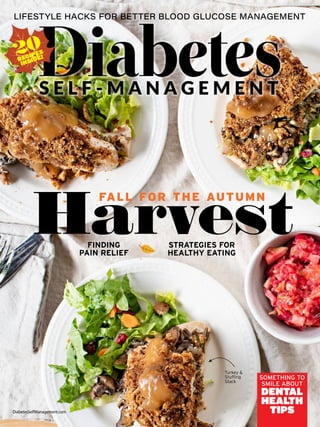
- 1. FINDING PAIN RELIEF STRATEGIES FOR HEALTHY EATING DiabetesSelfManagement.com SOMETHING TO SMILE ABOUT DENTAL HEALTH TIPS 20 RECIPES INSIDE! Turkey Stuffing Stack FALL FOR THE AUTUMN Harvest
- 2. 1. Kempf K, et al. Efficacy of the telemedical lifestyle intervention program TeLiPro in advanced stages of type 2 diabetes: A randomized controlled trial. Diabetes Care. 2017 Jul;40(7):863–871. 2. Lean M, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2017;391(10120):541–551. Groundbreaking Research Shows How to Regain Healthy Blood Sugar and Lose Weight One answer to healthy blood sugar levels is found in high-protein low-glycemic nutrition. People who live with diabetes want better options for getting a handle on their blood sugar, especially their HbA1c levels. The problem is that, even when we do try to eat right and exercise, our bodies still need extra help from our metabolism to light the fires of our glucose-burning furnace that’s nec- essary for weight loss. Knowing this, in 1985 German holis- tic therapist Hubertus Trouillé devel- oped a low-glycemic high-protein formula to be used as nutritional therapy by his patients living with di- abetes and slow metabolism. After following his dietary advice, Trouillé discovered that the formula not only helped his patients increase metabolism but also regain glycemic control and lose weight. Today, his unique formula, called Almased, has been scientifically studied for over 30 years. ADVERTISEMENT Study results show the Almased participants experienced: Weight loss Healthy HbA1c Reduced hunger Increased quality of life Healthy blood sugar Enhanced glucose handling and metabolism Low-Glycemic High-Protein Nutrition and Glucose Health In a 2017 study by Kerstin Kempf and a group of German researchers, a 12-week telemedical lifestyle inter- vention (TeLiPro) was carried out in patients with advanced type 2 diabetes.1 It included weekly phone calls by trained diabetes educators who talked about diet, exercise, and options for overall lifestyle changes. For the first 12 weeks, the TeLiPro group also received a low-glyce- mic high-protein dietary supple- ment — in place of three meals a day for the first week, two meals a day for weeks 2 to 4, then one meal a day for weeks 5 to 12. Time (Weeks) Mean Weight Loss (kg) Weight Reduction Weight Reduction Control Group TeLiPro Group
- 3. Nature has a solution and a cure for all of our problems. Taking guidance from mother nature, a manual has been created that helps cure Type-2 diabetes in a completely natural way, and its name is Diabetes Freedom. All one has to do is follow everything step by step from the Diabetes Freedom manual. Diabetes Freedom is available in e-form and can be downloaded on any of your devices. There will be no need to follow any exercise or diet plans; just through changes in diet patterns, one can avail of benefits. Click to Order Diabetes Freedom Program For an Exclusive Discounted Price
- 4. * Results are not typical. Individual results may vary based on starting weight and program adherence. These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease. Find Almased at these fine retailers! Made from high-quality soy, probiotic yogurt and enzyme- rich honey, Almased is diabetic-friendly — 27 on the Glycemic Index score. Almased can help: ○ Lower HbA1c and blood-sugar levels.* ○ Burn fat while retaining muscle.* ○ Aid the gut microbiome in supporting digestive and immune health.* ○ Curb cravings and support a healthy balance of the hunger hormones, leptin and ghrelin.* ○ Boost energy and support mood.* What makes Almased so different? Supported by over 30 years of scientific research. Unique fermentation process. All essential amino acids. Bioactive peptides. Honey-derived digestive enzymes. Vegetarian and gluten-free. No artificial fillers, flavors, sugars, preservatives or stimulants. The results? The HbA1c levels in the TeLiPro group were, on average, reduced by 1.1, from 8.4% to 7.3%. In this group, there were also signif- icant reductions in fasting blood glu- cose, body weight, body mass index, blood pressure, cardiovascular risk factors, and requirements for diabe- tes medications — a 20% lower need for medications and a nearly 50% re- duction in insulin needs. These improvements were even seen after 52 weeks of follow-up. There are other lifestyle intervention studies, with other diets, that have had some success, such as the 2017 DiRECT study in the U.K., which sug- gested that a very-low-calorie total diet replacement for up to 5 months, along with coaching by health prac- titioners, could achieve weight loss and reductions in HbA1c levels.2 But the U.K. study was hard to follow (25% dropped out), had some un- wanted side effects, and had a 2:1 ra- tio of carbs to protein. The Power of Almased The German researchers chose a formula that was high in protein (Almased) but low in carbohy- drates (nearly 2:1 protein to carbs), knowing that more protein in the diet naturally reduces insulin demand and increases fat burning. The takeaway from this research, and other published studies, is that while supporting glycemic control can be hard, it can be easier when our metabolism is working with us. The high-protein, scientifically proven, Almased Diet can help you reduce your HbA1c and blood sugar levels while sup- porting glycemic control. ADVERTISEMENT To learn more and to download your free diet plan go to almased.com/DM03E or call us toll-free at 1-877-256-2733 or e-mail us at info@almased.com.
- 5. Get tested for diabetic kidney disease If you have type 2 diabetes DKD can lead to kidney failure and dialysis and increases your risk for heart attack. DKD often has no symptoms until it’s too late, but when it’s caught early, there is more you can do to protect your kidneys. Ask your doctor for a UACR (urine albumin-to-creatinine ratio) urine test once a year. It checks for protein in the urine, one of the earliest signs of DKD or kidney damage. © 2021 Bayer Pharmaceuticals, Inc. All rights reserved. BAYER and the Bayer Cross are registered trademarks of Bayer. Last Updated 06/2021 PP-UN-CAR-US-0310–1 For more information, visit KidneyAlert.com or scan code Up to 40% of people with type 2 diabetes (T2D) develop diabetic kidney disease (DKD)
- 7. Dear Readers, Autumn is upon us, and with it have arrived all the changes this time of year brings: The weather is cool- ing down, leaves are turning vibrant colors, and shorts and tees have been exchanged for jackets and sweaters. Eager to usher in the season with some positive changes of your own? Read on. Blood glucose control is the cornerstone of diabetes management, and strategies such as regular monitoring, following a healthful meal plan, and getting regular physical activity are familiar steps that can help keep it in check. But there are a variety of other, less-well-known measures that can help, many of which you can start implementing today. Curious? Find out more in “Lifestyle Hacks for Better Blood Glucose Management” (page 24). If pain plagues your days, you may feel run-down and hopeless. But what you may not know is that pain and diabetes can be linked in a variety of ways, and there are approaches that can help bring relief. Learn about the connection between the two conditions and get helpful tips for managing pain at home in “Pain and Diabetes” (page 32). Remember, there is hope! Eating: It’s something we all do, but the trick is in knowing what and how much—often easier said than done. Indeed, whether you’re newly diagnosed or you’ve had diabetes for many years, this area of self- management can be challenging. Fortunately, there are some easy approaches that can get you on the right dietary path. Get started with the expert tips in “Strategies for Healthy Eating” (page 40). No matter what area of your management routine you choose to focus on in the coming months, you should be proud of all the hard work you’re putting in to stay healthy. Be well, and have a fantastic fall! All the best, Diane Fennell Editorial Director, Wellness Division ••• EDITOR’S NOTE ••• For customer service or subscription information, please call (855) 367-4813. ART PRODUCTION SeniorDesigner ScottBrandsgaard SALES MARKETING DirectorofMediaSolutions EdFeldman MediaSalesManager CheyenneCorliss ccorliss@madavor.com ClientServices clientservices@madavor.com MarketingDirector TimDoolan SeniorMarketingAssociate TommyGoodale SEOContentMarketingSupervisor AnthonyBuzzeo ContentMarketingAssociate SamanthaThomas CUSTOMER SERVICE CustomerService@DiabetesSelf-Management.us (855)367-4813 DiabetesSelf-Management, Fall 2021,Volume 38, Number 3. DiabetesSelf-Management (ISSN 0741-6253) (USPS 003-865) is published quarterly by Madavor Media, LLC, 35 Braintree Hill Office Park, Suite 101 Braintree, MA 02184. Periodicals postage paid at Boston, MA and at additional mailing offices. Copyright © 2021 Madavor Media, LLC. U.S. subscriptions $29.94 per year. Postmaster: Please send changes of address to Diabetes Self-Management, PO Box 460700, Escondido CA 92046. DiabetesSelf-Management@pcspublink.com. For customer service or subscription information, please call (855) 367-4813. Outside US: 760-496-7575. Advertising Sales: Madavor Media, LLC (800) 437-5828. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, elec- tronic or mechanical, including photocopying, recording, or any other means, without the prior written permission of Madavor Media, LLC. Statements and opinions expressed in this publication are those of the authors and not necessarily those of the publishers or advertisers.The purpose of this magazine is to provide readers with accurate and up-to-date medical information. It is not intended to provide medical advice on personal health matters, which should be obtained directly from a physician. We regret that we are unable to respond to inquiries about personal health matters. We sometimes make our list of subscribers available to carefully screened organizations whose products and activities may interest you.While many subscribers find this type of information valuable, some prefer not to receive unsolicited mail. Please contact our customer service department at (855) 367-4813 if you do not wish to receive such mailings. Photographs contained in this magazine are for illustration purposes only. OPERATIONS VP,CirculationStrategy JasonPomerantz SeniorClientServices OperationsLead AndreaPalli OperationsHumanResourcesCoordinator ToniEunice SeniorClientServicesMediaAnalyst TouZongHer ClientServices DarrenCormier AccountingDirector AmandaJoyce AccountsPayableAssociate TinaMcDermott AccountsReceivableAssociate WayneTuggle NewsstandDistributionWeeklyRetailService EXECUTIVE InmemoryofSusanFitzgerald,COO,1966-2018 SHUTTERSTOCK DIGITAL OPERATIONS AudienceDevelopmentAnalyst RyanGillis SeniorDigitalDesigner MikeDecker WordPressDeveloper DavidGlassman FoodEditor LorenaDrago,MS,RDN,CDN,CDCES EditorialDirector,WellnessDivision DianeFennell ChairmanCEO JeffreyC.Wolk ChiefOperatingOfficer CourtneyWhitaker ContentDirector MattMartinelli EDITORIAL BOARD PamelaAllweiss,MD,MPH CDCDivisionofDiabetesTranslation AmyP.Campbell,MS,RD,LDN,CDCES Boston,Massachusetts ShanaCunningham, MSN,RN,MLDE,BC-ADM,CDCES DiabetesEducationServiceCoordinator, UKHealthCareBarnstableBrownDiabetesCenter, UniversityofKentucky,Lexington,Kentucky RobertS.Dinsmoor SouthHamilton,Massachusetts DavidE.Goldstein,MD ProfessorEmeritus,UniversityofMissouri HealthScienceCenter,Columbia,Missouri LauraHieronymus, DNP,MSEd,MLDE,BC-ADM,CDCES,FADCES AssociateDirector,EducationQualityServices, UKHealthCare,BarnstableBrownDiabetesCenter, UniversityofKentucky,Lexington,Kentucky JeffPlumer,ViceChair, JDRFInternationalBoardofDirectors WilliamH.Polonsky,PhD,CDCES AssistantClinicalProfessor, DepartmentofPsychiatry, UniversityofCalifornia,SanDiego JeanneL.Rosenthal,MD AttendingSurgeon,RetinalService, NewYorkEyeandEarInfirmary,NewYork,NewYork GaryScheiner,MS,CDCES OwnerandClinicalDirector,IntegratedDiabetesServices, Wynnewood,Pennsylvania BernardP.Shagan,MD Director,DiabetesEducationCenter, MonmouthMedicalCenter,LongBranch,NewJersey RichardM.Weil,MEd,CDCES ExercisePhysiologistandDirector,MountSinaiSt.Luke’s WeightLossProgram,MountSinaiSt.Luke’s Hospital, NewYork,NewYork SusanWeiner,MS,RDN,CDCES,CDN,FADCES Owner,SusanWeinerNutrition,PLLC,LongIsland,NewYork StephenZ.Wolner,DDS NewYork,NewYork InMemoriamDr.LoisJovanovic,1947-2018 4 DiabetesSelfManagement.com • Fall 2021
- 8. E - C O U R S E TYPE 2 WELLNESS JOURNEY A 21-DAY E-COURSE SHUTTERSTOCK ••• DiabetesSelfManagement.com ••• NEWSLETTER Subscribe today for updates on diabetes news, research, recipes, weight management and more. bit.ly/2NDzTMz Sugar: Fact or Fiction A lot of misinformation surrounds diabetes, especially when it comes to sugar. How do you make sense of sugar in terms of what types and how much is“allowed”? Let’s clear up some of that confusion and set the record straight. bit.ly/34ce3Kd Type 2 e-Course If you or a loved one is living with type 2 diabetes, you probably have a lot of questions. Whether you’re brand new to the diagnosis or a seasoned veteran of dealing with the condition, our free e-course can help you find the information you need to live a happier, healthier life. bit.ly/3vbLDfk FREE PROGRAM Good-for-You Chicken Noodle Soup In the crisp days of fall, nothing hits the spot better than a steaming, hydrating bowl of chicken soup. Using skinless chicken breasts cuts down on the fat and calories in this low-carb version of the classic. bit.ly/3f5jukC RECIPE Hiking for Health If you’re interested in an active autumn, hiking might be just the exercise for you. Don’t be intimidated by the image of backpackers climbing the Rocky Mountains. The reality is that hiking can be as mild or rigorous as you choose. Get our tips for enjoying the great outdoors (and learn more on page 17)! bit.ly/3fuWo5K EXERCISE INTERACT WITH US Get more news, tools and recipes all month long! @ManageDiabetes @diabetesrecipes @DiabetesSelfManagement Are Beans Good for Diabetes? Beans have quietly risen to superfood status, thanks to their nutrition profile and low cost. You might be wondering if and how they can be part of your eating plan if you have diabetes. Are beans good or bad for blood sugars? Let’s take a look. bit.ly/3ue4bKx NUTRITION 6 DiabetesSelfManagement.com • Fall 2021
- 10. Fasting Glucose and Waist Size Predict Risk of Diabetes Complications BY QUINN PHILLIPS Fasting glucose level, waist cir- cumference and age at diabetes diagnosis are factors that help predict who will develop diabetes compli- cations, according to a new study published in the Journal of Diabetes and its Complications. Researchers looked at a diverse, multiethnic group of 1,587 partici- pants, all of whom had diabetes, in a study called the Multi-Ethnic Study of Atherosclerosis. Participants were divided into eight different groups based on three factors that split par- ticipants into two categories each.The first factor was age at diabetes diag- nosis, with participants divided based on an age of 45 or younger, or older than 45.The second factor was fasting glucose level, with participants divided based on a measurement of 140 mg/ dl or higher, or below this level. And the third factor was waist circumfer- ence, with women divided based on a measurement of 105 centimeters (41.3 inches) or greater, or below this level, and men divided based on a measure- ment of 110 centimeters (43.3 inches) or greater, or below this level. The researchers were interested in how each of these factors—age at diagnosis, fasting glucose level and waist circumference—was related to outcomes including death from all causes, cardiovascular disease, chronic kidney disease, heart failure, dementia and diabetic retinopathy (eye disease) during a follow-up period of about 17 years. In calculating how these factors were related to outcomes, the researchers adjusted for demo- graphic differences (like age or race), known behavioral differences, and known differences in clinical risk fac- tors (such as other health conditions). They found that the group of par- ticipants with both an early age at diabetes diagnosis and high fasting glucose experienced a higher risk of death, cardiovascular disease, heart failure, chronic kidney disease and retinopathy. The group with both an early age at diagnosis and a high waist circumference experienced a higher risk of cardiovascular disease, heart failure, chronic kidney disease and retinopathy. The group that had all three higher risk factors—early age at diagnosis, high fasting glucose and high waist circumference—experienced a higher risk of death, heart failure, chronic kidney disease and retinopathy. The researchers noted that these results reinforce the importance of assessing the risk for complications among people with diabetes based on their age at diagnosis, fasting glucose level and waist circumference—as well as the importance of using these findings to communicate with patients and to develop a strategy for prevent- ing diabetes complications. DSM ••• THE DOSE ••• News Notes SHUTTERSTOCK 8 DiabetesSelfManagement.com • Fall 2021
- 11. ••• THE DOSE ••• News Notes Too Many Older Adults May Be Taking Daily Aspirin BY QUINN PHILLIPS Two commonly recommended or prescribed drugs—daily aspirin and the cholesterol-lowering drugs statins—may not be taken by the right proportion of older adults, according to a new study published in the Jour- nal of the American Geriatrics Society. Both daily aspirin and statins have been shown to reduce the risk of car- diovascular events in some people, but they’re not recommended universally. Aspirin is generally recommended for adults with a moderate to high risk of developing atherosclerotic cardio- vascular disease (fatty deposits in the arteries) who have a remaining life expectancy of at least 10 years and are willing to take aspirin daily for at least 10 years. This means aspirin is most likely to be recommended for adults ages 50-59, with less evidence to sup- port its benefits for people ages 60-69. People under 50 or at least 70 are generally not considered candidates for daily aspirin without a history of cardiovascular disease (CVD). Statins, on the other hand, are gen- erally recommended at low to moder- ate doses for adults ages 40-75 who don’t have a history of CVD but who have one or more cardiovascular risk factors (such as diabetes, high blood pressure or abnormal cholesterol or triglyceride levels) and a moderate to high risk of developing atherosclerotic CVD.There isn’t enough high-quality evidence, the researchers write, to recommend that most adults over age 75 take either aspirin or a statin daily to help prevent CVD. Using data from the U.S. National Health and Nutrition Examination Survey (NHANES) between 2011 and 2018,the researchers looked at the use of both aspirin and statins in adults age 50 and older.They found that daily use of aspirin—mostly at low doses, as is recommended for preventive benefits— tended to increase with age and was quite similar across the range of years in the study.In 2017 and 2018,rates of daily aspirin use, almost always at the recommendation of a doctor, ranged from 20.0% in adults ages 50-54 to 49.6% in adults ages 70-74 to 53.7% in those age 75 and older. Daily use of statins also tended to increase with age,ranging in 2017 and 2018 from 17.8% in adults ages 50-54 to 47.7% in adults ages 70-74 to 52.3% in those age 75 and older.While these numbers are broadly similar to those for daily aspirin, the different clinical recommendations for each drug mean it’s likely that more older adults could benefit from taking statins than cur- rently take them—while it’s likely that too many older adults are taking daily aspirin and may be at higher risk for adverse effects like bleeding as a result. “Education...regarding the com- pelling benefits of using statins for the secondary prevention of CVD is important,” the research- ers wrote. Additionally, they note, “Healthcare providers should inform their older patients about the appropriate aspirin use.” DSM SHUTTERSTOCK 10 DiabetesSelfManagement.com • Fall 2021
- 12. Groundbreaking New Weight-Loss Drug Approved BY QUINN PHILLIPS The U.S. Food and Drug Admin- istration (FDA) has approved Novo Nordisk’s application to market a new formulation of the drugmaker’s type 2 diabetes drug Ozempic (semaglutide) as a once- weekly injection for weight loss. Sold under the brand name Wegovy, the new formulation for weight loss is a higher-dose ver- sion of Ozempic, a treatment to improve blood sugar levels that was approved by the FDA in 2017. Wegovy is intended to be com- bined with a reduced-calorie diet and increased physical activity to achieve weight loss in people who are overweight or obese, and who have medical problems related to their excess body weight. The new FDA approval is based on the results of a clinical trial called STEP (Semaglutide Treatment Effect in People with Obesity) that included about 4,500 participants. Trial par- ticipants who received Wegovy lost an average of 14.9% of their body weight over the course of 68 weeks, compared with 2.4% for participants who received a placebo (inactive treat- ment).What’s more, 83.5% of partici- pants in the Wegovy group lost at least 5% of their body weight, compared with just 31.1% who lost this much body weight in the placebo group. “This is the first time we have seen this magnitude of weight loss with a medicine,” said Rob- ert F. Kushner, MD, a professor of medicine and medical education at Northwestern Medicine’s Feinberg School of Medicine in Chicago. Wegovy should not be taken with any other products that contain semaglutide—such as Ozempic or Rybelsus—or any other drug in the GLP-1 receptor agonist family, which includes Trulicity (dulaglutide), Byetta and Bydureon (exenatide), Victoza (liraglutide), and Adlyxin (lixisenatide). Like many other drugs in this family, digestive upset is the most common category of side effects for Wegovy. DSM .((3,168/,122/ 6$)( 1R,FH3DFNV(YHU$JDLQ 7KH)5,2ŠLVDUHXVDEOHHYDSRUDWLYHFRROHUWKDW NHHSVLQVXOLQVDIHZLWKRXWHYHUQHHGLQJLFHSDFNV RUUHIULJHUDWLRQ HYHQLQWHPSVRIƒ)RUPRUH ‡ $FWLYDWHVZLWKZDWHU ‡ .HHSVLQVXOLQ%HWWDDQG9LFWR]DVDIHLQ KRWZHDWKHUIRUDSSUR[LPDWHOWZRGDV WKHQMXVWUHDFWLYDWH ‡ *UHDWIRUWUDYHO76$IULHQGO ‡ $0867IRUHPHUJHQFSUHSDUHGQHVV ‡ 6L]HVIRU9LDOV3HQV 3XPSV ‡ /RZFRVW 25'(572'$ ZZZ)5,2DVHFRP 63(,$/',62817283212'(³'60´
- 14. TYPE 1 DIABETES LINKED TO MUSCULOSKELETAL CONDITIONS BY QUINN PHILLIPS Type 1 diabetes is linked to a higher risk of developing musculoskeletal problems, including conditions like frozen shoulder and carpal tunnel syndrome, according to new research presented at the Diabetes UK Professional Conference (DUKPC) 2021. Researchers at the University of Exeter in England based their findings on an analysis of data from the UK Biobank—one of the largest general health studies in the world—and from FinnGen, a similar large study based in Finland. The researchers used both genetic information and health data to find out whether people with type 1 are at higher risk for a wide range of health conditions. They found that type 1 was likely to play a causal role in developing a range of musculoskeletal conditions, including frozen shoulder, carpal tunnel syndrome, trig- ger finger and Dupuytren’s contracture. Each of these conditions is marked by pain and reduced mobility in the shoulder, wrist, hand or fingers.They also found that type 1 was unlikely to play a causal role in developing osteoarthritis (the most common form of arthritis, in which joints degenerate). This study is the first large-scale analysis to show that type 1 diabetes is responsible for a higher risk of develop- ing musculoskeletal problems. Now that this connection is known, the researchers noted, people with type 1 and their doctors can be on the lookout for musculoskeletal problems that may develop as a result of diabetes. More research is needed, the researchers pointed out, to learn how diabetes and elevated blood glucose may contribute to the development of musculoskeletal problems. DSM PORTION CONTROL BY LISA CANTKIER Portion sizes matter when it comes to a healthy diet, particularly if you have diabetes. With obesity rates at an all-time high in the United States and around the world, we need to examine not only what we eat but also how much we eat. Odds are, your portion sizes may be larger than they should be. Find out what your portions should look like and how to truly take charge of your plate by taking this quiz. (Everyone is different, so be sure to ask your healthcare provider about your diet and meal portions to determine what is best for you.) 1.True/False:The“plate method”is a strategy that can help you achieve portion control. O OTrue O OFalse 2. Controlling the portions on your plate can: O OA. Result in healthy weight loss. O OB. Lead to a decrease in diabetes medication. O OC. Improve blood glucose control. O OD. All of the above. 3.Weight loss in people with diabetes who are over- weight is associated with which of the following? O OA. Decreased muscle tone. O OB. Normalized blood glucose levels and a reduced risk of other health problems. O OC. Increased LDL (“bad”) cholesterol. O OD. An increased risk of hypertension (high blood pressure). 4. Howcanyouestimateportionsizesforyourplate? O OA. Use measuring cups and measuring spoons. O OB. Use food scales. O OC. Use the palm of your hand, fist, fingers and thumb. O OD. Eyeball it. 5.True/False: Using a smaller plate size does not help control meal portions. O OTrue O OFalse QUIZ See page 14 for answers. SHUTTERSTOCK ••• THE DOSE ••• News Notes 12 DiabetesSelfManagement.com • Fall 2021
- 16. American Lung Association’s LUNG FORCE, Amgen, Cless Family Foundation, Fanconi Anemia Research Fund, Farrah Fawcett Foundation, Jazz Pharmaceuticals, Laura Ziskin Family Trust, Legacy Circle, LUNGevity Foundation, Mirati Therapeutics, Pancreatic Cancer Canada, Sara Schottenstein Foundation, Society for Immunotherapy of Cancer, Lew, Jean, and Kari Wolff Stand Up To Cancer is a division of the Entertainment Industry Foundation (EIF), a 501(c)(3) charitable organization. SATURDAY 8/21 8 ET/7 CENTRAL CANCER DOESN’T STOP. NEITHER DO WE. FOR ONE NIGHT. WE STAND TOGETHER.
- 17. ••• THE DOSE ••• News Notes REDUCED-CARBOHYDRATE, HIGH-PROTEIN DIET SHOWS BENEFITS IN TYPE 2 BY QUINN PHILLIPS Following a reduced-carbohydrate, high-protein diet may provide a variety of benefits to people with type 2 diabetes, including better glucose control and reduced hunger, according to a small study published in theAmeri- can Journal of Physiology-Endocrinology and Metabolism. The study’s participants were 28 adults with type 2 diabetes, who were randomly assigned to follow either a reduced-carbohydrate, high-protein diet or a conventional diabetes diet for six weeks.The reduced-carbohydrate diet got 30% of its calories from carbohydrate,30% from protein and 40% from fat, while the conventional diabetes diet got 50% from carbohydrate,17% from protein and 33% from fat. The researchers found that following a reduced-car- bohydrate, high-protein diet resulted in total after-meal glucose elevation (“area under the curve”) that was 60% lower on average, as well as 24-hour glucose levels that were 13% lower, compared with the conventional diabetes diet. Participants’ after-meal insulin secretion rate was also 24% lower, while pancreatic beta cell sensitivity to insulin increased by 45% on this diet. Stomach empty- ing was delayed by an average of 15 minutes, while self-reported fullness between meals increased by 18%. These results show dramatic benefits, and no sig- nificant disadvantages or risks, linked to following a reduced-carbohydrate, high-protein diet in a small group of people with type 2 diabetes. “It is noteworthy that these results were achieved in a setting that aimed at body weight maintenance,” rather than weight loss, the researchers wrote—suggesting that the difference in diet composition, rather than a reduction in overall calories, was responsible for the benefits observed. Based on these results, the researchers concluded, many people with type 2 diabetes may benefit from a modest shift in their diet composition away from carbo- hydrate and toward protein. DSM SHUTTERSTOCK 1.True. According to the American Diabetes Associa- tion, the“plate method”can help you create“perfectly portioned meals with a healthy balance of vegetables, protein and carbohydrates without any counting, calculating, weighing or measuring…all you need is a plate.”This method suggests you fill one-quarter of your plate with protein, one-quarter with whole grains or other whole-food carbohydrates, and half with colorful nonstarchy vegetables.The recom- mended beverage of choice for the plate method is filtered water. Avoid processed foods. 2. D. Portion size is an important determinant of energy intake. In people with type 2 diabetes, weight reduction improves blood glucose control. According to research, portion control tools are effective in lead- ing to weight loss and enable people with diabetes to decrease their blood glucose medications without sacrificing glycemic control. 3. B. According to Diabetes Canada,“Portion size is an important part of weight loss. If you’re overweight or obese, weight loss is the most important and effec- tive way to help normalize blood sugar levels and reduce your risk of other health problems.”DC says you should fill half your plate with vegetables and fruits.The organization also notes that“Low-glycemic- index foods such as legumes, whole grains, and fruits and vegetables can help control blood sugar...and can make you feel full longer to help with losing weight.” 4. A, B, C. Measuring cups and spoons and food scales are useful tools for determining portion size.The Cen- ters for Disease Control and Prevention teaches people how to estimate portion size using their hands when these tools aren’t available. For example, 3 ounces of meat, fish or poultry = the palm of the hand (no fin- gers), 1 cup or 1 medium fruit = a fist, 1 tablespoon = a thumb tip (tip to first joint), 1 teaspoon = a fingertip (tip to first joint). 5. False. The results of a study in the journal BMC Obesity showed that using a plate smaller than a tra- ditional dinner plate resulted in participants consum- ing smaller food portions.This is an effective strategy you can try to help manage your portions. (Just be mindful that portion control plates have the potential to reduce portion sizes of important items—if you try this, don’t skimp on your nonstarchy veggies!) DSM LisaCantkierisawriterandeducatorspecializinginnutri- tion and health. She is coauthor of the diabetes-friendly cookbook The Paleo Diabetes Diet Solution. QUIZ ANSWERS See page 12 for questions. 14 DiabetesSelfManagement.com • Fall 2021
- 18. ••• THE DOSE ••• Product Spotlight Philips SmartSleep Sleep Wake-Up Light If the longer nights have you yearning for more time in bed, maybe it’s time to treat yourself to the gift of healthy sleep. The Philips SmartSleep Sleep Wake-Up Light is a sound investment in your health.You can customize your nighttime and morning routines with sunset and sunrise simulation, which allows you to wake up more naturally using a combination of light and sound.This device also provides an FM radio, a reading lamp with 10 brightness settings and a tap snooze in case you want to sleep a bit longer. Fall asleep faster and wake up feeling energized. usa.philips.com Cool New Products to Try BY AMY CAMPBELL, MS, RD, LDN, CDCES Tea Forte Single Steeps Tea Chest Sampler There are so many reasons to enjoy a hot cup of tea. Some are health-related, including a lower risk of heart disease, type 2 diabetes and some types of cancer, and less depression and anxiety. Drinking a cup of tea can also help you unwind from a busy day or let you catch up with a good friend. Whatever your reasons are, you’ll be sure to appreciateTea Forte’s Single SteepsTea Chest Sampler.You’ll get to experience a wide range of different teas (28, to be exact) from around the world. Fix yourself the perfect cup of tea anytime, anywhere withTea Forte’s single-serve pouches. teaforte.com Quility Weighted Blanket For people with diabetes, constant stress and lack of sleep can make it harder to manage blood sugars. A quick and easy way to improve your sleep and banish stress is to use a weighted blanket. Weighted blankets, such as the Quility Weighted Blanket, provide the right amount of pressure on your body—much like getting a good hug. This blanket is made from high-quality, durable materials, including microglass beads and a removable, breathable duvet cover.You’ll feel comforted and relaxed, and you’ll finally get a good night’s sleep without getting overheated. quilityblankets.com Fall 2021 • DiabetesSelfManagement.com 15
- 19. Diabetes Freedom – What is it all about? A large amount of the population today suffers from the deadly disease called diabetes; especially Type-2 diabetes is becoming a common problem among the population. A large number of diabetic patients get their legs amputated. Many times, diabetic patients are left helpless because there seems to be no cure for their condition. They can only survive if they take their medications on time. Their bodies get so used to the support from these tablets that the body’s ability to function on its own is diminished. For years people have been dealing with type-2 diabetes, but no permanent cure still exists for the condition. Or is the world being fooled by all the big drug companies and manufacturers? There are natural ways through which one can bring under control one’s blood sugar level.
- 20. Hypoglycemia Defined, Hidden Carbs BY GARY SCHEINER, MS, CDCES ••• THE DOSE ••• Ask Away SHUTTERSTOCK QMy lab work says that a blood glucose level in the 60s mg/ dl is normal, but I’ve always been told that anything below 70 mg/dl is too low. Which is correct? AThere is a great deal of debate in the medical/scientific world about the true definition of hypogly- cemia (low blood glucose). For anyone at risk of hypoglycemia, including those who take insulin or medications that increase insulin production, the general rule has always been that anything below 70 mg/dl is considered too low and should be avoided. Glu- cose levels below 70 mg/dl will usually cause the body to produce adrenaline, which leads to the classic symptoms of hypoglycemia (e.g., shaking, sweat- ing, rapid heartbeat, intense hunger). While these symptoms can be unpleasant and disruptive, they are not necessarily dangerous. Research has shown that, for most people, the mind and body can still function rea- sonably well even with glucose levels in the 60s. However, once glucose dips below 55 mg/dl, things change dramatically. At this point, the brain lacks the energy to function prop- erly. Confusion can set in, and it may become difficult or impossible to eat or drink something to treat the low. And some people experience this at levels higher than 55 mg/dl. Given how quickly glucose can drop, most people aim to keep their levels from going below 70 mg/dl. Think of glucose levels in the 60s as a guardrail that keeps you from fall- ing over a cliff. You’re safe as long as you stay behind the guardrail, but if you push against it too hard or lean too far over it, you can easily wind up falling into a pit of doom. Best to have a discussion with your diabetes care team to determine precisely how low is too low for you. QThe other day, all I had for lunch was a salad with some cashews. Within a few hours, my blood glucose had risen almost 100 mg/dl! Why would it rise so much if I didn’t have any sugar or starch? AWelcome to the world of “hidden” carbohydrates. Many people think the only sources of blood- glucose-raising carbs are obvious foods such as bread, potatoes, fruit and sweets. But there are carbs in almost everything we eat. Salads, for example, contain an average of about 4 to 5 grams of carbohydrate per cup. And cooked nonstarchy vegetables, such as steamed broccoli, contain 8 to 10 grams per cup. A handful of cashews contains about 10 grams of carbohydrate, and a handful of peanuts contains roughly 6 grams (of course, handful sizes may vary!). Milk is another source of carbs—about 12 grams per cup. And that doesn’t even touch on sauces, dressings and condiments. A single tablespoon of barbecue sauce can contain 5 to 10 grams of carbohydrate! There are a few exceptions. Most meats, eggs and cheeses are com- pletely carb-free. But carbs may be added during food preparation. It pays to look up the contents of your common meals and snacks to make sure your carb counts match what you actually consume. DSM Gary Scheiner, MS, CDCES, has lived with type 1 diabetes for 30 years and was named Diabetes Educator of the Year 2014 by the Association of Dia- betes Care Education Specialists. Have a question about diabetes? Email gary@integrateddiabetes.com. 16 DiabetesSelfManagement.com • Fall 2021
- 21. Take a Hike! BY ROB DINSMOOR I’ve always enjoyed hiking, but I especially came to love it during the pandemic because it gave me an excuse to leave my house, breathe fresh air, and enjoy the scenery. If you haven’t hiked before, it’s never too late to begin. Hiking can increase stamina, improve bone density, strengthen leg muscles, strengthen your core, and improve your bal- ance. It can also help you control your weight, improve blood pressure, lower blood glucose levels, and gener- ally reduce the risk of heart disease. A wide variety of fancy gear is marketed to hikers, but all you really need to start out is a lightweight back- pack and sturdy, durable hiking boots that fit well. (I remember hiking in old boots that seemed to be made of lead, but there are many lightweight yet durable options available today.) Hiking poles are also recommended, especially on hills, because they help you keep your balance, particularly going downhill, and take some of the stress off knees and hips. What do you put in your backpack? Water is the most important item, since hiking inevitably builds a thirst, and there are usually no water foun- tains or convenience stores in the wild. It’s also prudent to carry blood glucose monitoring supplies and snacks and/ or glucose tablets in case of hypogly- cemia (low blood glucose). If there’s any chance of being out after dark, definitely pack a flashlight. All geared up with nowhere to go? Members of the Appalachian Mountain Club (outdoors.org) have access to organized hiking trips and related events. The Hiking Project (hikingproject.com) offers maps for hiking trails all over the world and allows you to search for trails near you. Meetup.com has regional hiking groups that provide group hikes, most of which are free to members. Most if not all states have hiker-friendly state parks and forests, often with large trail maps on display and smaller trail maps that you can carry. The U.S. Forest Service (fs.usda.gov) has a searchable database of forests and grasslands in various states. For people who prefer flat sur- faces, consider abandoned railroad tracks that have been converted to hiking and biking trails, offering natu- ral scenery you can’t usually see from the road. Over 22,000 miles of trails in the U.S. alone have been converted by the Rails-to-Trails Conservancy (railstotrails.org), which can give you information about converted rails in your state. I also enjoy walking on nearby beaches, some of which go on for miles—and if I want a more intense workout, I hike up and down the dunes. Safety is particularly important when you’re starting out. It’s a very good idea to hike with a friend, so you can help each other if one of you gets hurt. You should also stay on marked paths and trails. Check the weather forecast so you can dress accordingly, especially if there is likely to be cold weather or rain. Above all, have fun! DSM ••• THE DOSE ••• Curmudgeonly Athlete SHUTTERSTOCK Fall 2021 • DiabetesSelfManagement.com 17
- 22. It is easy to get caught up in the widespread mentality that we should move in only certain ways. Some advocates for specific types of exercise—yoga, strength training, running, you name it—will encour- age you to “just do this, it’s the only workout you need!”You can be sure this is a marketing gimmick, and unfortunately, it gives a false impres- sion of what our bodies actually need. So, what should we be doing, then? Our bodies are dynamic, versatile and always adapting to what we do often (even if we don’t do it well). In other words, we should move in all the ways available to us (or, as the popular meme goes, do ALL the things). If you were to step into a yoga class, your instructor might suggest you position your body in particular ways to “accomplish”different poses. What they may not tell you is that each body on each mat should look different. This is the same for gener- ally all types of movement: We each have a unique skeleton that directly influences our ability (or inability) to move, shift and bend. (That does not mean, however, that maintaining proper alignment is not important.) There are fundamental movement patterns that most people’s skeletons are generally able to achieve. Skeletal variations such as where your hip socket sits in your pelvis (which varies greatly from person to person) and many other structural differences determine how you are able to move and how you will be able to optimize a particular movement. Exploring new movements can help you learn what is best for your unique body. In Western society, there is a det- rimental and often dangerous fixa- tion on the way things look. We are obsessed with symmetry, which is ironic considering that our bodies are built asymmetrically (e.g., we have a heart on one side, a liver on one side, and so on).This asymmetry alone creates a cascade of structural “misalignments” from the ribcage to the pelvis and to the joints beyond. With all that being the case, why then should we move in just one way? The answer is, we shouldn’t. Our bod- ies are built for and crave a variety of types of movement, and there is not a single “magic” way to train that is for everyone. Exploring new patterns of movement and incorporating variety into your routine can help reduce your risk of overuse injuries from repeating the same things over and over (even sitting can cause overuse injuries). Try these simple and fun move- ments to notice your own imbalances and add some diversity to your physi- cal activity regimen. DSM Laurel Dierking, MEd, NASM, 700- ERYT, is a movement specialist with a concentration in yoga, strength con- ditioning, exercise physiology and postural restoration. With 10 years of extensive experience, Dierking seeks to enhance self-awareness by guiding individuals through mindful movement, functional training,body awareness and breath work. Move In All the Ways BY LAUREL DIERKING, MED, NASM, 700-ERYT ••• HEALTHY LIVING ••• The Right Moves SINGLE LEG CHAIR TO STAND • Sit in a secure chair with your spine tall and your heels under your knees. • Extend one leg off the floor (for more support, extend the leg while keeping the heel on the floor). • Without using your hands (unless you have to), come up to a standing position using just your one leg. • Slowly, with control, return back to your seat, still with just the one leg. • Repeat five to 10 repetitions on each leg. ARMS OVER HEAD AND SHAKE • Set a timer for 1 minute. • Stand with your feet hip-width apart or wider, reaching your arms overhead. • Begin to gently bounce in your legs and shake your arms vigorously overhead. • Breathe steadily as you shake and bounce your limbs. • After 1 minute, gently bring your arms down beside you and relax your posture, returning your breathing to normal (in and out through the nose). SINGLE LEG REACHES • Stand on one leg next to a desk or a wall in case you need support (perform this exercise with no support for a challenge, but have support nearby). • Keep your knee straight (but not locked) and hinge (on an exhale), folding from your waist to reach as far forward in front of you toward an object as you can. Keep your back leg reaching back. • Inhale and come right back up to standing. Repeat 10 times on each leg. 18 DiabetesSelfManagement.com • Fall 2021
- 23. AARON ASHLEY Fall 2021 • DiabetesSelfManagement.com 19
- 25. ••• HEALTHY LIVING ••• Weighty Matters SHUTTERSTOCK 4 Ways to Healthy Habits BY DR. NICOLA DAVIES, PHD Fall conjures up images of moun- tains of roasted turkey, fresh- baked pumpkin pie and bright candy apples—none of which are ideal for weight management! Fortunately, though, the season has many redeem- ing features that can help you get closer to your health goals. Indeed, the good news for people with diabe- tes is that studies show blood glucose levels are typically lower during the autumn months. Here are a few tips for embracing the fall to accelerate your healthy habits. Recognize and manage mood dips. Experts recog- nize that, with less daylight and the stress of the looming holiday season, fall can cause mood dips. Being on a strict diet can worsen these dips, making you feel con- stantly “hangry.” One tried-and- tested weight-management strategy that can help avoid low moods is being mindful of what you are eat- ing. Don’t deny yourself food—sim- ply replace empty calories with healthier options. Replace chips with baked crackers or plain popcorn, for example. If you crave bread, go for a whole-grain, low-glycemic version. Keep track of your intake using an app. Above all, slow down and enjoy your food. Harness the power of healthy fall foods. The autumn harvest is perfectly suited for those looking to embrace a healthy diet. You can use pump- kin, broccoli and butternut squash to make warming, hearty soups that are low in calories. Fresh apples and pears can satisfy sweet crav- ings. Other filling fall produce, such as cauliflower and Brussels sprouts, can be included in your meal plan to help you keep the weight off without feeling hungry. (Read “Making the Most of Autumn” [page 22] for some more inspiration.) Gear your exercise rou- tine to the fall weather. Fall weather motivates people to get moving.The chillier temperatures and colorful outdoors can make exer- cising a pleasure. Take advantage of this by planning hikes along scenic trails or jogging through your local park. Fall is also a great time to get into sports with family and friends— lacrosse, baseball or football are just a few ideas. Stay active indoors. Yes, sometimes the air may be just too chilly for you to enjoy the outdoors. However, staying indoors doesn’t mean you need to give up your exercise routine. There are a variety of ways to bring your exer- cise inside—consider yoga, aerobics or even dancing. There are plenty of fitness apps and videos available online to help you stay fit without leaving the house. In it for the long haul Weight management needs to be a long-term lifestyle change rather than something that comes and goes like the seasons. Tweaking your usual habits this fall may help you avoid “holiday weight” altogether. DSM Dr. Nicola Davies, PhD, health psychology, is the author of I Can Beat Obesity! Finding the Motivation, Confidence and Skills to Lose Weight and Avoid Relapse. 2 3 4 1 20 DiabetesSelfManagement.com • Fall 2021
- 26. SMART Tabatchnick Balsamic Tomato Rice Soup 1 pouch 100 530 0 20 4 4 3 Amy’s Black Bean Vegetable Soup 1 cup 210 540 0 35 7 4 9 Pacific Foods Organic Cashew Carrot Ginger Bisque 1 cup 140 570 3.5 22 4 11 2 Bar Harbor Rhode Island Style Clam Chowder 1 cup 140 570 1 19 0 1 9 Pacific Foods Organic Chicken Wild Rice Soup 1 cup 120 610 1 16 2 2 5 Campbell’s Well Yes! Garden Vegetable With Pasta, Lightly Salted 1 cup 90 640 0 18 3 5 3 Campbell’s Well Yes! Chicken Noodle Soup 1 cup 110 640 0.5 13 2 2 8 SMARTER Healthy Choice Vegetable Beef 1 cup 120 400 0.5 20 3 4 7 Campbell’s Chunky Healthy Request Split Pea Ham Soup 1 cup 150 410 0.5 24 5 3 12 Pacific Foods Organic White Bean Kale Millet Soup Made With Chicken Bone Broth 1 cup 130 430 1 18 3 1 10 Pacific Foods Organic Creamy Golden Cauliflower Soup 1 cup 120 450 3 13 2 5 4 Progresso Light Beef Pot Roast Soup 1 cup 70 470 0 9 1 2 5 Healthy Choice Chicken With Rice Soup Made With Chicken Bone Broth 1 can 110 480 0 12 2 1 11 Progresso Reduced Sodium Hearty Minestrone Soup 1 cup 120 480 0 21 4 4 5 SMARTEST Tabatchnick Split Pea Soup, Low Sodium 1 pouch 180 35 0 33 13 5 12 Health Valley Organic Minestrone Soup 1 cup 100 45 0 18 3 5 4 Health Valley Organic Chicken Noodle Soup, No Salt Added 1 cup 80 130 0 13 1 1 5 Imagine Butternut Squash Creamy Soup, Light in Sodium 1 cup 100 230 0 21 2 7 1 Amy’s Organic Minestrone Soup, Light in Sodium 1 cup 120 270 0 18 4 4 4 Dr. McDougall’s Right Foods French Lentil Soup, Lower Sodium 1 cup 130 280 0 24 9 3 8 Amy’s Organic Fire Roasted Southwestern Vegetable Soup, Light in Sodium 1 cup 140 340 0.5 20 4 4 4 RECOMMENDED SERVING CAL SODIUM SAT FAT (g) CARBS (g) FIBER (g) SUGAR (g) PROTEIN (g) Soup BY AMY CAMPBELL, MS, RD, LDN, CDCES Chosen wisely, soup is a great way to sneak in some vegetables, whole grains and even an ounce or two of protein. Homemade soup is generally your best nutritional option, but the reality is that store-bought soups are a mainstay for many of us—they’re quick, convenient and easy to prepare. The downside of store-bought soups? Sodium, and lots of it. Excess sodium contributes to high blood pressure, stroke and heart attack. Luckily, there’s a decent assort- ment of store-bought soups that are reasonable (and even low) in sodium and that are tasty, too! Choose soups with less than 480 milligrams (mg) of sodium, less than 5 mg of saturated fat, and at least 3 grams (g) of fiber per serving. If possible, look for at least 7 g of protein per serving, too. As for higher-sodium soups? Enjoy them in moderation and limit your portion (go for a cup rather than a bowl). DSM SHUTTERSTOCK ••• HEALTHY LIVING ••• Smart Smarter Smartest Fall 2021 • DiabetesSelfManagement.com 21
- 27. Autumn is upon us! What are the best ways to incorporate fall har- vest fruits and vegetables into a healthy meal plan for managing diabetes? One way to create natural variety in your eating pattern is to change your produce selection based on the season. What is seasonally available will vary somewhat regionally,but this roundup includes commonly available fall produce, along with tasty ways to add these items to your diet. (Each person with diabetes needs to decide how to incorporate various types of produce into their meal plan and recognize that while nothing is completely off-limits,portions and pro- duce choices may impact blood glucose levels in different ways.The way foods are paired with fats and proteins can slow digestion and also minimize a postmeal rise in blood glucose in some cases.Speak with a registered dietitian about the best produce picks and pair- ings for your meal plan.) APPLES NUTRITION FACTS: MEDIUM: CALORIES: 104, FAT: 0.0 G, PROTEIN: 0.5 G, CARBOHYDRATE: 28.0 G, FIBER: 4.8 G Baked Apples. Bake apples with cinnamon, walnuts and raisins. Breakfast Apple Quesadilla. Spread your favorite nut butter on a low-carbohydrate wrap and add thinly sliced apples. SavoryApple Coleslaw/Salad.Add sliced apples to coleslaw and salads. Butternut Squash and Apples. Bake butternut squash and apples with your favorite fall spices or combine for a savory-and-sweet soup. Homemade Applesauce. Use your favorite recipe for homemade apple- sauce to add to pancakes and muffins, or simply enjoy with a sprinkle of cin- namon for a snack. BEETS NUTRITION FACTS: 1 CUP: CALORIES: 77, FAT: 0.0 G, PROTEIN: 2.8 G, CARBOHYDRATE: 17.0 G, FIBER: 5.0 G Berry Beet Smoothie. Combine frozen berries,½ cup of pine- apple or banana, cooked beets and yogurt (or a nondairy option) for a simple refreshing smoothie. Roasted Beet Side Salad. Roast fresh beets and drizzle with balsamic vinegar and top with 1 ounce of feta or crumbled goat cheese. Strawberry and Beet Ice Pops. Combine frozen strawberries, ½ cup of cooked beets, nondairy milk, pure vanilla extract and sweetener to taste. Put mixture in a popsicle mold and freeze for two to three hours, until frozen. Pickled Beets. Look for a no-sugar pickled beet recipe or reduce the sugar in your favorite recipe for a tangy treat to top salads or eat as a simple side dish. Raw Beet Salad. Grate raw beets and add shredded carrots, onions and your favorite vinaigrette. COLLARD GREENS NUTRITION FACTS: 1 CUP, COOKED: CALORIES: 44, FAT: 0.8 G, PROTEIN: 4.0 G, CARBOHYDRATE: 8.0 G, FIBER: 5.5 G Braised Collard Greens. Use veg- etable or chicken stock and water to cook collard greens over low heat in a covered pot. Add red pepper flakes, garlic,or lemon juice and zest for flavor. Collard Slaw. Thinly slice collard greens, purple cabbage, carrots, red onion or any vegetables of choice to create a custom collard slaw to treat your taste buds.Dress with your favor- ite creamy slaw dressing. Shredded Collard Green Salad With Roasted Vegetables. Remove stems and thinly shred collard greens for the salad base.Top with your favor- ite fall roasted vegetables,such as sweet potatoes or butternut squash. Add 1 ounce of goat cheese and lightly salted nuts or seeds for added texture, flavor and protein. Skillet Greens With Ham. Pan-fry collard greens with onion, garlic, and Canadian bacon or ham. CRANBERRIES NUTRITION FACTS: 1 CUP, RAW: CALORIES: 46, FAT: 0.0 G, PROTEIN: 0.0 G, CARBOHYDRATE: 12.0 G, FIBER: 3.6 G Cranberry and Orange Relish.Try making a no-sugar-added cranberry sauce by combining fresh cranberries, 1 navel orange, fresh orange zest and sweetener of choice (to taste) in a food processor. Pulse until the mixture is chunky but without large pieces. Fresh Cranberry Chutney and PorkTenderloin.Combine fresh cran- berries, apples or pears, and spices to create a fragrant and flavorful chutney to use with pork tenderloin or turkey. Cranberry and Orange Parfaits. Layer low-fat yogurt with 2 tablespoons of fresh cranberry sauce and sliced oranges and top with 1 to 2 table- MakingtheMostofAutumn Meal and snack ideas BY ALISON MASSEY, MS, RD, LDN, CDCES ••• HEALTHY LIVING ••• Food For Thought SHUTTERSTOCK 22 DiabetesSelfManagement.com • Fall 2021
- 28. spoons of chopped nuts for a quick snack or breakfast. Cranberry Applesauce. Consider adding some fresh cranberries to your next batch of homemade applesauce for a tangy-sweet combination. GRAPES NUTRITION FACTS: 1 CUP, FRESH: CALORIES: 104, FAT: 0.0 G, PROTEIN: 1.0 G, CARBOHYDRATE: 27.0 G, FIBER: 1.3 G Roasted Grapes and Brussels Sprouts. Toss Brussels sprouts in olive oil and sprinkle with salt and pepper. Bake in a preheated oven at 450°F for about 20 to 30 minutes. In a saucepan, add grapes, thyme and 1 to 2 tablespoons of butter. Cook until grapes are glazed. Pour mixture over prepared Brussels sprouts. Pecan Chicken and Grape Salad. Prepare chicken salad as usual and add toasted chopped pecans and fresh sliced grapes. Jell-O Frozen Grapes.Wash grapes (don’t dry).Empty a sachet of sugar-free Jell-O powder into a bowl. Roll grapes in the Jell-O powder until coated.Place the Jell-O-covered grapes in a single layer in a freezer-safe container and freeze for at least 1 to 2 hours. Balsamic Grape Crostini. Toss grapes in 1 to 2 tablespoons of olive oil to coat and bake in a preheated oven at 375°F for about 15 minutes.Use warm grape topping on pre-prepared warm French baguette slices and drizzle with balsamic vinegar. PARSNIPS NUTRITION FACTS: 1 CUP, COOKED: CALORIES: 146, FAT: 4.5 G, PROTEIN: 2.0 G, CARBOHYDRATE: 26.0 G, FIBER: 5.6 G Roasted Parsnip “Fries.” Wash and peel parsnips. Slice lengthwise into strips and coat with olive oil,finely chopped rosemary and a sprinkle of salt and pepper. Bake in a 450°F pre- heated oven for about 20 minutes, or until the parsnips are tender and slightly browned. Mashed Parsnips and Carrots. Wash and peel parsnips and carrots. Steam for about 15 to 20 minutes, or until the vegetables are tender. Place the carrots and parsnips into a food processer and add ½ tablespoon of olive oil, orange zest, salt and pepper. Process until the vegetables reach a creamy texture. Parsnip“Rice.”Wash and peel pars- nips.Slice into large cubes and add to a food processor.Pulse until the parsnips reach a rice-like size. Sauté the riced parsnips over medium heat for about 8 minutes when ready to use. PEARS Baked Pears With Walnuts. Pre- heat oven to 350°F. Cut pears in half and place on a baking sheet. Use a melon baller and scoop out the seeds. Sprinkle each ½ pear with walnuts, cinnamon and a drizzle of maple syrup or honey. Bake for about 30 minutes. Ricotta Toast With Sliced Pears. Combine ricotta, orange zest and 1 teaspoon of maple syrup or sweet- ener of choice. Spread ricotta mixture on toast. Top with ½ ripe sliced pear and sprinkle with toasted almonds or walnuts. RUTABAGAS NUTRITION FACTS: 1 CUP, COOKED: CALORIES: 72, FAT: 0.0 G, PROTEIN: 2.0 G, CARBOHYDRATE: 16.0 G, FIBER: 4.0 G Mashed Rutabagas.Boil rutabagas and then mash with butter or olive oil as you would potatoes. Rutabaga Oven “Fries.” Wash and peel rutabaga and slice into strips. Coat in olive oil and toss with your favorite seasonings, such as cayenne, salt, pepper or garlic powder. Roast in a preheated oven at 425°F for about 30 minutes. Raw Rutabaga Salad. Shave or grate rutabaga and carrots and add sliced scallions. Toss in your favorite vinaigrette dressing. TURNIPS NUTRITION FACTS: 1 CUP, COOKED: CALORIES: 34, FAT: 0.0 G, PROTEIN: 1.0 G, CARBOHYDRATE: 8.0 G, FIBER: 3.0 G Parmesan Turnip Chips. Using a mandolin, slice turnips as thinly as possible. Toss turnip slices in olive oil and sprinkle with salt. Lay turnip slices on a baking sheet and bake in a preheated oven at 425°F for about 30 to 35 minutes, until the chips are cooked evenly. Sprinkle the baked chips with grated parmesan cheese. Turnip-Potato Mash. Place peeled and chunked turnips and potatoes into boiling water. Cook for about 20 min- utes, or until the potatoes and turnips are easily pierced with a fork.Drain the turnips and potatoes in a colander and return to the pot.Blend the turnips and potatoes with an immersion blender until they are a creamy consistency (add milk or nondairy milk and butter, as you would during the preparation of mashed potatoes). WINTER SQUASH (ACORN) NUTRITION FACTS: 1 CUP, CUBED: CALORIES: 115, FAT: 0.0 G, PROTEIN: 2.0 G, CARBOHYDRATE: 30.0 G, FIBER: 9.0 G Baked Acorn Squash. Bake acorn squash and use to top salads or a win- ter slaw. Acorn Squash Purée.Bake or steam acorn squash and then purée and add a pinch of cinnamon or nutmeg.Add to your pasta sauce or soups for a boost of extra nutrition. Casseroles/Vegetable Lasagna. Add baked or roasted acorn squash to any of your favorite casseroles or even a vegetable lasagna. DSM Alison Massey, MS, RD, CDCES, is a registered dietitian and certified diabetes educator in Maryland. She blogs at amassey.com. Fall 2021 • DiabetesSelfManagement.com 23 NUTRITION FACTS: 1 CUP, FRESH: CALORIES: 71, FAT: 0.0 G , PROTEIN: 0.0 G, CARBOHYDRATE: 19.0 G, FIBER: 3.8 G Poached Pears. Bosc pears are the best choice for poaching. Pears can be poached in a liquid of choice, such as apple cider or red wine. Look for a recipe that suits your tastes and adjust any added sugars to best fit your goals for your eating plan.
- 29. 24 DiabetesSelfManagement.com • Fall 2021 24 DiabetesSelfManagement.com • Fall 2021
- 30. Diabetes Freedom Worth Buying? Reviews – Can George Reilly James Freeman’s Main Manual control your blood sugar level naturally?
- 31. Lifestyle Hacks for Better Blood Glucose Management BY GILLES BEAUDIN, CSEP-CEP, MSc SHUTTERSTOCK Fall 2021 • DiabetesSelfManagement.com 25 Fall 2021 • DiabetesSelfManagement.com 25
- 32. Many health conditions are mul- tifactorial, meaning that there’s usually more than one cause, and diabetes is no exception. Most people with type 2 diabe- tes know how important regulating their carbohydrate intake and getting enough exercise are for managing their diabetes. Recent research has found that other lifestyle modifications can also have a positive influence on blood glucose levels.These modifica- tions involve: • EXERCISE INTENSITY • EXERCISETIMING • SLEEP • COLD EXPOSURE • GUT BACTERIA What’s more, the impacts of these lifestyle hacks are not limited to glu- cose control. They will benefit many aspects of your life. If you are curi- ous, read on. You will discover how you can incorporate them into your daily routine. EXERCISE INTENSITY Work a little harder, sometimes. You hopefully have a regular exercise routine. If you don’t, you may have the same reason as most nonexercisers: lack of time.But recent research shows that you can get a lot of benefits from short training sessions. The secret? Work a little harder, in intervals. In studies, increasing the intensity of exercise has resulted in similar or better metabolic improvements than longer, less-intense routines for people with type 2 diabetes, all in a fraction of the time. Part of the reason is that higher intensities use more muscle fibers, which in turn use more glucose. In fact, your muscles are respon- sible for clearing the majority of the glucose from your blood. To make them more sensitive to insulin,you just need to reduce their glucose stores. Because higher-intensity exercise requires more muscle fibers to be used, this reduces the glucose stores in more fibers. A review article published in 2015 reported that interval walking (alternating intervals of fast- and slow-paced walking) better improves glycemic control in people with type 2 diabetes than consistently paced walking that uses a similar amount of energy. This indicates that how many calories you burn matters less than how you burn them. If more of those calories come from glucose, it will have a bigger effect on blood glucose control. How to up your intensity. Evi- dence shows that interval training is generally safe and has metabolic benefits for those with type 2 diabetes. After getting the go-ahead from your doctor,it is important to progress grad- ually and ease into higher-intensity intervals.As you get better, you can go a little harder. Just give your body a chance to adapt. If you exercise a few times a week, only try higher-intensity intervals twice a week to start. It’s not necessary to incorporate them into every exercise session. The intensity of your intervals will depend on your level of fitness and tol- erance. If you are a beginner, walking faster for 30 to 60 seconds during a stroll may be a good place to start.This is equivalent to what fitness expert Covert Bailey called wind sprints: small modifications in intensity that will challenge your wind. One word of caution: Before your exercise session, check your blood glucose. If it is over 240 mg/dl, check your urine for ketones. If you have ketones, do not exercise, as this could make your glucose go even higher. EXERCISETIMING When you exercise. Now that we have established that it matters how hard you exercise, the question is: Does it matter when you exercise to improve your glucose control and/or insulin sensitivity? Studies have shown that the peak in blood glucose happens around 90 minutes after the start of a meal. Making storage space for glucose in your muscles by being physically active is the best way to reduce that peak, and exercising within 30 min- utes of a meal is the best way to maximize the effects of your training session. That goes for any type of exercise. Also, it has been reported that exercising after meals is more effective than exercising once a day for blood glucose control in people with type 2 diabetes. How to time exercise. Glucose from a meal starts to trickle into your blood roughly 15 minutes after you start to eat. Exercise will open up space in your muscle fibers, making them more responsive to the effects of insulin. If you can change the tim- ing of your exercise sessions, give it a try. Here’s my rule of thumb: Try to exercise 30 minutes before or after a meal. If your preference is shorter, higher-intensity workouts, I would suggest you exercise before your meal. High-intensity activities after eating may disturb your digestion. But there’s nothing wrong with a brisk walk after a meal. SLEEP ON IT Researchers are learning more about the effects of not getting enough restful sleep.And that’s a good thing: Sleep is one aspect of wellness that doesn’t get its fair share of attention.The Centers for Disease Control and Prevention (CDC) call insufficient sleep a public health epidemic. Experts generally recommend that healthy adults sleep seven to nine hours a night, but about 35% of Americans report typically sleeping less than seven. Sleep deprivation has been linked to a variety of metabolic dysfunctions, including reduced insulin sensitivity. Even one night of four hours’ sleep can decrease insulin sensitivity. Six nights at this rate will drop your insu- lin sensitivity by 24%.And don’t think that you can compensate for it on the weekend: Running a sleep deficit during the week and sleeping in on the weekend will not readjust your insulin sensitivity. Do you find it hard to resist your cravings?Your willpower may not be to blame. Sleep deprivation will also disturb certain appetite hormones, which will make you hungrier. How’s that for a double whammy? How to get more sleep. When it comes to the influence of sleep on blood glucose control, recent evidence suggests that lifestyle modifications 26 DiabetesSelfManagement.com • Fall 2021
- 33. are better than relying on medica- tion in order to regulate appetite and glucose metabolism. Get into a sleep routine: Go to bed and wake up at the same time each day. Also be aware that light sends the message that it is time to get up. Dim the lights and stay away from screens at least 30 minutes before bed, and use light-blocking shades to make your room as dark as possible, so you don’t get woken early by the sunrise. Here’s an extra trick—you can boost melatonin naturally by practicing deep breathing. Researchers reported a reduction in stress hormones and an increase in melatonin from deep diaphragmatic breathing. Doing this before bed will help improve the qual- ity of your sleep. Try this: Lie down on your back, knees bent and feet flat on the floor. Put one hand on your chest and the other on your belly, below the ribs. Take a deep breath and make the hand on your belly move up.The one on your chest should stay stable.Take three to four seconds to breathe in and six to eight seconds to breathe out. You want to feel your lower ribs expand. That rib expansion is from the contraction of your diaphragm. Practice this until it becomes a smooth flow in and out. COLD EXPOSURE Turn on your furnace. Your body always aims for a state of homeostasis, or balance.That includes maintaining a certain body temperature.When the environmental temperature drops, your body has mechanisms in place to maintain its own temperature. One of those is activating a type of fat that is known as brown adipose tissue (BAT). This tissue is like a mini furnace, using energy to create heat. In people used to living in temperature-controlled environments, it gets activated less, just like an unused muscle. Research shows that by exposing your body to a colder environment, you will get BAT to take up glucose and fatty acids to crank up the heat. A review article published in 2016 concluded that mild cold exposure is a good strategy for the prevention and treatment of type 2 diabetes. How to master cold exposure. One word of caution: Cold exposure is like exercise for your blood vessels. It makes them contract. Check with your doctor before trying this, particularly if you have a heart condition. Also, if you are a beginner, don’t push too hard. Your body is adaptable, but it needs time to make adaptations, so go at it easily. If you live in a part of the world that gets cold winters, you can drop the thermostat a few degrees. You can also slowly get used to taking a shower with colder water. Start your shower as usual.After washing your- self, gradually lower the temperature of the water. Get used to colder water every week, just for one to two min- utes. You will eventually “train” your BAT to become more active. GUT BACTERIA Trust your gut. This is fairly new knowledge, and we don’t know all the details, but the evidence is too strong to ignore. The gut is often referred to as the second brain. Its nervous system is very complex, and it secretes certain substances that have influences on other body tis- sues. The data in humans are still scarce, but an article published in 2019 reported that certain bacteria that populate your gut could influence insulin resistance. In fact, the link between the two appeared very strong, and it was shown that people with type 2 diabe- tes have a lower count of certain gut bacteria. Is this just a link, or does one cause the other? That remains to be determined. How to adjust your gut. Fortu- nately, there’s no need to wait for the answer.A healthy gut is important to your overall health. It has been shown that certain pesticides can reduce your good gut bacteria, and the use of antibiotics can ravage your intestinal flora.To rebuild it, eating foods rich in prebiotics (food for your gut’s healthy bacteria)—such as onions, garlic and leeks—and probiotics (health-pro- moting bacteria and yeasts)—such as those found in yogurt, kefir and sauerkraut—can be helpful. Also, eat a variety of fresh foods, favor high-fiber vegetables and fruits, and eat organic when you can. And as much as possible, stay away from processed products. (Sound familiar? Healthy eating has many benefits.) Take the first step As Albert Einstein wisely said, “The definition of insanity is doing the same thing over and over again but expect- ing different results.” That applies to your social circle, your family life, your financial position and your health. If you want to see a change, you need to change your habits. In most cases, lifestyle modifica- tions work well. They are not always easy because they involve changes to the way you live, and they tend not to work as quickly as medications. But they are always the right thing to do. Give your body what it needs, and you will see results. DSM Gilles Beaudin, CSEP-CEP, MSc, is a clinical exercise physiologist at Cleveland Clinic Canada. Sleep deprivation has been linked to a variety of metabolic dysfunctions, including reduced insulin sensitivity. Fall 2021 • DiabetesSelfManagement.com 27
- 34. As you are probably aware, diabe- tes is best managed with a team approach. Your team includes your diabetes medical providers (physi- cians, nurse practitioners and physi- cian assistants), diabetes care and education specialists, dietitians, exer- cise experts, nurses, pharmacists, mental health professionals and, most importantly, you! But did you know that your team should also include dental specialists? It is important to establish an ongoing relationship with a dental hygienist and dentist for your oral health care.Your dental hygienist will conduct a professional cleaning and provide instruction on routine home care and cleaning to maintain or reestablish oral health, while your dentist will perform an oral examina- tion and diagnose conditions such as cavities, gum disease, and yeast and/ or fungal infections. As part of your care, you should also receive an oral cancer screening during a dental visit. In fact, taking care of your mouth and teeth is a big part of your diabetes health. It is very important to make every effort to ensure you keep up your daily oral hygiene practices and schedule regular visits with your den- tist and dental hygienist for cleanings and oral health checkups. Your dental toolkit A healthy mouth begins with proper maintenance. Always keep a tooth- brush and toothpaste on hand. Brush your teeth at least twice a day, in the morning and evening, ideally after meals and snacks. Soft-bristled tooth- brushes are best to clean the teeth and along the gum line. Hard or firm bristles can irritate your gums and cause them to recede (or pull away from the teeth) over time. Make sure your toothbrush is in good condition, with bristles that are not bent or frayed. Be certain to replace your toothbrush about every three months.Your tooth- brush should be a comfortable size for your mouth. A toothbrush that is too big can make it hard to reach all tooth surfaces and limit your range of move- ment—the ability to move the tooth- brush around—while brushing. Whether to use a manual or an electric toothbrush is up to you. How- ever, your dentist or dental hygienist might suggest an electric toothbrush if they see you are having trouble cleaning thoroughly with a manual brush. If you start to use an electric brush, you will likely be asked to bring it to one of your office visits so the hygienist can show you how to use it based on the design. To use a manual brush, you should hold the toothbrush at an angle and brush your teeth with short circu- lar strokes, being sure to cover all sur- faces of the teeth, including the gum line. When using an electric brush, most of the movement is done for you, but you’ll still want to work with your dentist and hygienist to make sure you’re getting the best possible results. Remember, the goal of brushing is to remove food debris and the “sticky” plaque that can be easily missed along the gum line. Brushing all of your teeth should take about two minutes. Flossing and cleaning between your teeth is especially important and is recommended as a daily practice.Your dentist or hygienist will help determine what type of floss or flossing device is best to clean these hard-to-reach areas. Flossing is a learned skill, and the selection of the best interdental cleaner should be recommended by the dentist or hygienist, with one-on- one instruction provided for how to use it. While dental floss is the best choice for many people, other tools, such as preloaded floss on a dental pick, interdental brushes or Stim- U-Dents, might work better for you. These tools help break up and remove plaque and trapped food that the toothbrush can’t reach. Your dentist or hygienist can help you learn how to floss or show you how to use one of the other interdental cleaning tools to make it easier if you have arthritis or difficulty moving your hands. You should practice good dental care on a daily basis and schedule a visit with your dentist and hygienist at least twice a year for a cleaning and oral health checkup. Diabetes and dental disease People with diabetes are at higher risk for dental complications. These include gum disease, tooth loss and dry mouth that could cause thrush or other infections.TheAmerican Dental Association says that one out of five cases of tooth loss is connected to diabetes, and that 22% of people with diabetes have gum disease. If you have diabetes and are a smoker, the risk for gum disease is 20 times higher. Hyperglycemia and your mouth Hyperglycemia (high blood glucose) can make dental problems much worse.When blood glucose levels are consistently high, the glucose in your saliva also increases, which provides “food”to the harmful bacteria in your mouth, helping it grow. In addition, consuming foods high in sugars and starches can make your saliva thick and add to the growth of bacteria, which increases the amount of plaque. Plaque is a soft, sticky film that can be found most commonly at the gum line. If plaque is not removed by proper brushing and flossing, it can turn into DentalDefinitions Gingivitis: Red, swollen and bleeding gums caused by inflammation from plaque. Periodontitis: Gum disease caused by infection in the gums, which can lead to irreversible damage to the teeth, bone and tissues. Plaque: Sticky film along the gums containing bacteria. Tartar: Hardened plaque that has not been removed. Thrush: A naturally occurring fungus that grows uncontrollably, causing white patches in the mouth that may progress to open sores. Also known as candidiasis. Xerostomia: Lack of saliva in the mouth, or“dry mouth,” which can lead to pain, cracked lips and mouth sores. 30 DiabetesSelfManagement.com • Fall 2021
- 35. tartar, which is hard and can’t be removed with routine brushing and flossing. Tartar can only be removed by your dentist or dental hygienist. Plaque and tartar buildup that is not removed can lead to swollen, inflamed gums that become tender, red and bleed easily. This condition is called gingivitis, and 50% to 90% of people worldwide have it, but it is reversible. However, a condition called peri- odontitis is not reversible, and it can develop if your gingivitis is not treated. Periodontitis is a chronic gum disease that causes the gums to pull away from the teeth and form spaces, or “pock- ets,” around the teeth. These pockets collect food debris and bacteria and limit your ability to clean your teeth at home.Without proper cleaning, these pockets can become infected.As these infections spread between teeth and under the gum line, they can begin to damage the bone and gum tissues that support the teeth. This can lead to loose teeth, difficulty chewing and eventual tooth loss. Periodontal dis- ease is a risk associated with diabetes. Some studies have shown that screen- ing for diabetes in dental offices has resulted in up to 30% of individuals being diagnosed with prediabetes or diabetes when referred back to their primary care provider. Bleeding and inflamed gums can be a window into what is happen- ing to the rest of the body. Bacteria from infected gums can move into the bloodstream with normal activities like eating, flossing or brushing your teeth. Once these bacteria enter the blood- stream, they can start a chain reaction in the body’s defense system, which can trigger problems in the mouth and throughout the rest of the body. This increase in the defense system can have harmful effects and lead to more inflammation,which could cause blood glucose levels to climb even higher by making your body more resistant to insulin. In addition, the higher blood glucose can delay healing of wounds and infections, which can increase your risk for gum swelling and bleed- ing gums, increased pockets and bone damage, and certain infections. Hyperglycemia can also increase your risk for dry mouth and an oral fungal infection called thrush (also known as candidiasis).Hyperglycemia can cause dry mouth by decreasing the production of saliva,which is one of the body’s natural weapons to protect your oral health. Saliva washes away food debris and it also dilutes the harmful acids from food and bacteria.Without enough saliva, bacteria and acids can build up and lead to tooth problems and gum disease. Thrush is caused when a fungus that normally occurs in the mouth begins to grow uncontrol- lably.Sore white or red patches can be found on the roof of the mouth, gums, tongue and cheeks, causing pain and discomfort, especially with eating and drinking.Medication can be prescribed by your dentist or diabetes care pro- vider to treat thrush.Your toothbrush (as well as anything that touched your mouth during the outbreak) should be replaced. Good news Research shows that thorough, rou- tine dental cleaning at home and regular dental checkups can ensure optimal oral health by reducing inflammation of the teeth and gums and actually improving blood glucose levels in people with type 2 diabetes. Treatment of severe gum disease in people with type 2 diabetes has been shown to lower A1C levels (a long-term measure of glucose con- trol), with the benefit being about the same as you might experience if your diabetes care provider added another diabetes medication. Now that is something to smile about! DSM Korinne Callihan is a doctor of nursing practice student at the University of Kentucky College of Nursing. Dawn Dawson is a registered dental hygienist and certified clinical research coordinator at the University of Kentucky College of Dentistry. Laura Hieronymus is a doctor of nursing practice, master licensed diabetes educator, and the associate director of education and quality services at the UK Barnstable Brown Diabetes Center. StayonTrack You can do many things to limit your risk of dental problems. If you have diabetes and are concerned about your oral health, consider these tips to keep you on the right track: • Stay connected with your diabetes care provider and diabetes care and education specialist for optimal blood glucose control. • Keep your gums as healthy as possible at home by using good dental care practices. • Check your mouth often for any signs of red, swollen or bleeding gums. • Be sure to visit your dentist at least twice a year and ask the hygienist to discuss the measures they take to check your gums for pockets and any signs of damage. • Plan for your visit! Contact the dental office ahead of your appointment to discuss your medications and how long the visit will take, so you can plan around meals. •Take your diabetes medicine and eat your meals on your regular schedule. If your medicine can cause hypoglycemia (low blood glucose) or if the visit will interfere with your mealtime, plan to bring a snack or source of treatment to the office with you. • Have your blood glucose monitor on hand to check your levels before the dental visit and while you are there, if necessary. •Talk to your diabetes care provider and your dentist about the best way to prepare for your appointment. • Finally, if you smoke, work with your diabetes care provider to make a plan to quit. Smoking increases your risk for gum disease, oral and throat cancers, and fungal infections in the mouth like thrush. Smoking also raises your risk for many other diabetes- related complications. Fall 2021 • DiabetesSelfManagement.com 31
- 37. 32 DiabetesSelfManagement.com • Fall 2021
- 38. Pain and Diabetes What’s the connection, and how to get relief BY ALICIA DOWNS, RN, MSN, CDCES Diabetes is a chronic, lifelong condition, so it’s not sur- prising that it both impacts and is impacted by so many areas of our lives. It can also be associated with its share of stigma, and people living with diabetes may hear things like “Just do what your doctor says, and it will get better” or “You can change it if you really want to.”These messages can wear us down and leave us feeling hopeless. Similarly, pain can be a chronic, lifelong condition. For some, pain comes and goes, but for others, it is a part of every day. As with diabetes, pain conditions can impact many areas of our lives and can also be associated with stigma. Fall 2021 • DiabetesSelfManagement.com 33
- 40. The combination of having to man- age pain and having to manage diabe- tes can feel overwhelming, and some may react by avoiding dealing with either one. You may be surprised to learn, though, that your diabetes and your pain may be linked in a number of ways, and improving your care and management in one area can improve the other. Let’s dive into how diabetes and pain are linked and learn about some ways to get relief. The link between diabetes and pain Diabetes can directly affect our experi- ence of pain. Studies have shown that elevated blood glucose levels reduce our body’s pain suppression mecha- nisms. In other words, the chemical, neurological and hormonal processes that should reduce our experience of pain are inhibited. There is also evi- dence that when blood glucose levels are elevated, pain medications may be less effective.People with diabetes may therefore need additional assistance with pain management. Muscles and joints. Diabetes can also cause changes in our bodies that are painful.The muscles and joints are two of the most commonly affected areas. These issues often start with postural or movement injuries that lead to loss of flexibility. This loss of flexibility leads to tension, stress on joints, and pressure on nerves, which can be very painful.This pain, in turn, then leads to less movement and less flexibility. Eventually, muscles can shorten or even atrophy (waste away), and the cycle is very hard to break. Did you know that elevated blood glucose levels also cause loss of flex- ibility? When there is excess glucose in our blood, the connective tissues (tendons and ligaments) that hold our muscles and bones together and keep our joints in alignment get gly- cated (linked with sugar molecules). As a result, they become more rigid and less flexible, which adds pain to everyday tasks and can make being active less enjoyable. Nerves. Another pain condition experienced by many people with dia- betes is a long-term complication called neuropathy (nerve damage). Damage from high blood glucose levels to the small blood vessels leads to reduced circulation to nerve fibers. Without sufficient oxygen and nutrients, these nerves begin to die. Nerve damage can cause numbness, and it can also be extremely painful. (Anyone who’s had a hand or foot“fall asleep”and felt the pins and needles of nerves briefly deprived of oxygen flow has an inkling of the pain potential of nerve damage.) PAD. People with diabetes are also at higher risk of developing periph- eral arterial disease (PAD), a condition in which arteries become blocked and circulation is reduced. When PAD affects the legs, symptoms can include TipsandTechniquesforManagingPain What can we do to help manage pain? Prescription medication options can be effective, but they also carry risks and the potential for side effects. Before we look to steroids, opiates, nerve blocks and other medicines and procedures, what can we do to help reduce and manage our pain issues at home? Here are a few suggestions. (Be aware that, because pain can increase blood glucose levels, starting pain management can result in low blood glucose, or hypoglycemia. A reduction in insulin or other blood- glucose-lowering medications may be needed at the start of treatment, so work with your healthcare team to have a plan in place.) Avoid injury. Maintain a healthy weight, since carrying extra weight increases the risk of joint and back injury and pain. Also adopt a stretching routine. Maintaining flexibility reduces strain on joints and nerve pressure, so stretch daily. Be sure to stretch both before and after exercise to avoid muscle and joint injuries. Consider hot and cold therapy. Talk to your doctor about the use of hot and cold therapy to relieve pain, particularly muscle pain. From heating pads and hot water bottles to cold compresses and cooling sprays, these therapies can reduce inflammation, improve circulation, reduce swelling and increase comfort. Try physical therapy/chiropractic care. Don’t think of these as another appointment; think of them as a personal trainer your insurance will pay for! Physical therapy can help you increase range of motion and flexibility. Your therapist can give you exercises to strengthen muscles and reduce the burden on painful joints. They can even help you find patterns of misuse that have been leading to your pain in the first place. Physical therapy is available and covered by insurance for nearly any cause of pain, and coverage is often continued until the issue is resolved. These professionals can also guide you in the use of stimulation therapy.This involves using a device that emits a low electrical impulse, which can help block pain receptors if worn long-term. Some versions can even be implanted for pain management. In shorter-term use, this treatment creates tiny micromovements in the muscles that can help them release tension and increase circulation to reduce pain and nerve impingement. Get moving to stay moving. It may hurt to get moving at first, but the more we move, the less it will hurt. So, while an injury may have us briefly sidelined while healing, it should never stop us from moving entirely. As we move, circulation increases, helping muscles to receive oxygen and nutrients and heal better, reducing fluid in joints that causes painful stiffness, and allowing muscles 34 DiabetesSelfManagement.com • Fall 2021
- 41. pain in the calves, thighs and hips, which typically occurs with activity and goes away with rest. Blood glucose and pain The risk of developing these painful complications can be reduced by keeping blood glucose levels in tar- get range and taking steps to avoid erratic blood glucose swings. This can be complicated, however, since not only does diabetes impact pain, but pain can impact blood glucose. Why is this? For one thing, when we are in pain, it is hard to maintain regular physical activity, which in turn makes it harder to keep blood glucose levels stable and in target range. Experiencing pain can also raise our levels of stress hormones, which increase insulin resistance and elevate blood glucose levels. Inflammation from a chronic injury can also cause persistent low-level elevation in blood glucose. In these cases, diabetes medications may need to be increased to keep blood glucose levels well-managed. Additionally, people who live with chronic pain are also far more likely to self-medicate with food—rates of food addiction and binge eating dis- orders are much higher in those who report chronic pain—and to deal with depression. People in pain are also more likely to miss or cancel health- care appointments, which leads to a general reduction in overall wellness. If we struggle due to the burdens presented by a pain condition, our diabetes may take a back seat. So, as we can see, managing pain is not just important for quality of life—it can actually be a critical com- ponent of diabetes management, too See the tips and techniques below to help you get started. There is hope I live with chronic pain, and I live with diabetes. Managing both of these conditions together is key to staying healthy and active and enjoying life. Just as it is for you, it is important that I work with my entire medical team to achieve my goals and to ensure they under- stand how my pain control and blood glucose management are equally important and depend on one another. With good communica- tion and a collaborative approach, you can feel better. DSM Alicia Downs, RN, MSN, CDCES, is the director of patient care and education at Integrated Diabetes Services in Wynnewood, Pennsylvania. After an initial diagnosis of type 2 diabetes,she was diagnosed with LADA (latent autoimmune diabetes in adults) and uses her personal experience and diverse nursing background to coach people with diabetes. Visit integrateddiabetes.com to learn more. to strengthen and stabilize injured areas. It may ache to get started, but remember that the more we move, the less we hurt.Work with your doctor on a plan to manage that initial pain and ensure you can get moving without further injury. Stretching is a fantastic place to start! Investigate topical options. Topical pain relievers can be effective for muscle pain and short-term relief. Options include menthol gels, magnesium oil sprays, lidocaine and numbing creams.These great options are available over the counter, cheaply and without sedative or digestive side effects (be aware, though, that too much magnesium can cause loose stools) or the potential for addiction.Topical pain relievers are of minimal assistance for more severe nerve pain or joint pain, but they can provide temporary relief to assist in mobility. Look into over-the-counter medications. Speak with your provider about the use of over-the-counter medications.While these options can be highly effective, using them long-term can pose some potential health risks (such as liver function issues from acetaminophen or blood pressure and digestive impacts from long-term NSAID use).They may also interact with other medications you take. However, these medicines can be highly effective for treating pain. A recent study even showed that alternating acetaminophen and ibuprofen every four hours resulted in pain control comparable to opioid pain management.Talk with your prescriber about appropriate use, timing and dosages to meet your needs. Fall 2021 • DiabetesSelfManagement.com 35
- 42. 36 DiabetesSelfManagement.com • Fall 2021 36 DiabetesSelfManagement.com • Fall 2021
- 43. HowAm I Going to Remember to Do That? 8 strategies to manage your daily diabetes regimen BY SUSAN WEINER, MS, RDN, CDCES, FADCES, AND LESLIE JOSEL D o you feel pressure trying to remember everything you need to do to manage both your busy life and your diabetes? You are not alone! Juggling your daily dia- betes to-do list along with home and family responsibili- ties, plus school and work, can overwhelm even the most organized person. Although life is filled with unexpected distractions, we believe you can create systems and strate- gies that can help streamline your diabetes management. SHUTTERSTOCK Fall 2021 • DiabetesSelfManagement.com 37
- 44. Here are eight surefire tips and tools to help get you started. 1.WHAT’S YOUR STYLE? Recognize how you prefer to remem- ber to do things and tap into the prac- tices that work for you. For example, perhaps you like your reminders fun and visual, so leaving yourself col- orful notes on your bathroom mir- ror (e.g., to remember to check your blood sugar or pack your lunch) might work for you. If you are comfortable and familiar with technology and find the alarms and alerts from an insulin pump or continuous glucose monitor (CGM) useful, then timers and smartwatches that also use alarms as reminders may be the way to go. It doesn’t matter what your personal style is, as long as it helps to get those memory juices flowing. PROTIP: If you spend a good part of your day in front of your computer, set alerts for to-dos on your desktop calendar. Notifications will pop up on your screen without making any noise, so your work or virtual meetups won’t be disrupted. 2. ROUTINE, RITUAL, REPEAT. The beauty of routines or rituals is that they take away the need to “remember to remember.” Think of a routine as something that needs to be planned only once. It provides the ability to move through your tasks without thinking about what’s next. Think about the routines and ritu- als you already have in place that are working for you. Perhaps you always charge your phone in the kitchen and never forget it since you pass through that room often. Or you leave your diabetes supply bag by the front door, so you literally must step over it to leave your home. If you have a system or routine that is already working for you, pairing it with another task you want to remember may be an easy way to adopt an additional routine.For example, if you never miss your morn- ing brew, place your oral medications or pill box in your“coffee drawer,”and voilà! Every morning you will be pre- sented with a gentle visual reminder to take your medication. PROTIP: One of our favorite apps for habit building is The Habit Hub. It’s customizable and encourages you to create daily habits by reminding you to perform your tasks and track- ing when you complete them. The app creates a visual “chain” when tasks are completed; as the chain gets longer, it serves as an incentive for you to keep at the task so you don’t break the chain. 3. PUT THE ITEM FRONT AND CENTER! If you are prescribed oral medications (or routinely take vitamin and mineral supplements), you can use the bottles or containers as a visual reminder. ALERTSAND REMINDERSFOR PEOPLEWHO AREHEARING IMPAIRED • For iOS, turn on the“LED Flash for Alerts”feature. Go to Settings Accessibility Hearing Audio/ Visual. The phone will flash with a bright light when you have a notification (such as a programmed CGM alert). • For Android, turn on the“Flash Notification.”Go to Settings General Accessibility Hearing. • While sleeping (or when you may not be able to look at your device), wear your smartphone on an armband and enable the vibration feature. SHUTTERSTOCK 38 DiabetesSelfManagement.com • Fall 2021